
 |
|
|||||||
| Sexual Health Issues If you need medical advice regarding your sexual health, ask Dr Tan. We are honored to have an In House Doctor who is here to help. |
 |
|
|
Thread Tools |
|
#211
|
||||
|
||||
|
Re: Sexual Health News
Small penis syndrome: Everything you need to know
By Zawn Villines https://www.medicalnewstoday.com/articles/324569.php People with small penis syndrome do not have a physical condition but experience persistent anxiety about the size of their penis. These individuals worry that their penis is too small or that others will judge them for its size. Some doctors refer to small penis syndrome as penile dysmorphic disorder (PDD), but the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) does not list PDD as a separate disorder. Instead, it includes PDD as a variant of body dysmorphic disorder (BDD). What is small penis syndrome? People with small penis syndrome or PDD do not have an unusually small penis. Instead, they are severely anxious about their penis size. Having a small penis is not a medical diagnosis. Very rarely, a person's penis is small enough to interfere with sexual functioning, and doctors will refer to it as a micropenis. People with a micropenis have a penis that is at least 2.5 standard deviations smaller than the average penis. PDD is a type of BDD, which is a disorder that distorts a person's perception of their body. BDD can trigger immense anxiety in a person about their appearance. People with PDD feel shame and anxiety about penis size. They may mistakenly believe that they have a micropenis, even when their penis size is normal. Average penis size statistics Estimates on average penis size vary. Many people believe that a typical penis is 6 inches (in) long, but this is false and misleading, potentially triggering anxiety in those who worry about having a small penis. A 2014 analysis of data from 15,521 men discovered the following about penis size: The average non-erect penis is 9.16 centimeters (cm), or 3.61 in long. The average erect penis is 13.12 cm (5.17 in) long. Penises longer than 6 in when erect are rare, with this length of penis falling in the 90th percentile. Other research has sought to quantify what counts as a micropenis. A 2014 study defined a micropenis as a penis that is less than 7 cm (about 2.75 in) in length when flaccid and stretched. Furthermore, research on more than 52,000 heterosexual men and woman found that 85 percent of women were satisfied with the size of their partner's penis. In comparison, only 55 percent of men were satisfied with their penis size. Symptoms It is common for people to occasionally worry that their penis might not be large enough, especially when they feel pressure from the media and from seeing larger male genitals in pornography. However, people with small penis syndrome obsessively worry about penis size. Some symptoms of small penis syndrome or PDD include: constantly comparing their penis size to that of others, including those in the media a belief that the penis is unusually small, in spite of evidence to the contrary distorted perceptions of penis size placing an unusually high value on penis size feeling ashamed or embarrassed about penis size difficulty having sex with a partner because of anxiety about penis size reduced sexual function, including getting an erection or having an orgasm Some people with small penis syndrome have other symptoms of BDD. These might include: obsessive preoccupation with appearance repetitive or compulsive behavior relating to appearance, such as grooming or buying clothes chronic distress about appearance depression or anxiety about appearance Although small penis syndrome and BDD might appear to be the same condition, there are essential differences. Small penis syndrome is not a medical diagnosis, whereas doctors can diagnose a person as having BDD. Treatment For people with mild-to-moderate anxiety about penis size, researching data on average penis sizes or asking a doctor about what constitutes a micropenis may help. If a person is concerned about sexual performance, they may find comfort from a partner's reassurance and support. Research suggests that the majority of heterosexual women are satisfied with their partner's penis size. Medical treatment can help men with BDD or anxiety about penis size. Some treatment options include: Cognitive behavioral therapy (CBT): This type of therapy helps people understand how their thoughts affect their feelings and behavior, and it can help them find ways to reduce anxiety. Understanding and addressing triggers. For some, specific triggers — such as pornography or relationship problems — can cause penis size anxiety. Some people can reduce symptoms by identifying their triggers and working to manage them. Sex therapy or couples counseling. When penis size anxieties affect a person's relationship or ability to have sex, therapy can help a couple work together to overcome the anxiety. Questions to ask a doctor People who worry about the size of their penis or their feelings about penis size should see a doctor for help and support. Some questions to ask include: Is the size of my penis within the average range? Is it common to be anxious about penis size? What can I do to overcome my anxiety? Can you refer me to a therapist? Do I have symptoms of BDD? Are there effective strategies for managing sexual dysfunction relating to anxiety? Summary Anxiety relating to penis size can be frustrating, and it may affect self-esteem and relationships. Misconceptions about penis size can lead people to believe that their penis is smaller than most other people's, even when it is within the average range. Sex education, support from a partner, and appropriate treatments can help people with small penis syndrome and those with BDD manage their anxiety. |
|
#212
|
||||
|
||||
|
Re: Sexual Health News
What causes pain in the penis?
By Beth Sissons https://www.medicalnewstoday.com/articles/324608.php Many conditions can cause penis pain, and it can range from mild to severe. Pain may occur at rest, during sexual activity, or when urinating. While a person can sometimes get relief from penis pain at home, some underlying causes may need medical treatment. This article looks at the possible causes of penis pain, as well as the additional symptoms and treatment options for each. Causes of penis pain include: Peyronie's disease Peyronie's disease occurs when scar tissue creates plaque that builds up on the top or bottom of the penis. The cause of Peyronie's disease is still unclear, but doctors believe it to be a result of scarring to the penis. Scarring may be due to an autoimmune disease or a severe or repeated injury to the penis. Symptoms of Peyronie's disease include: erectile dysfunction or pain during an erection pain during sex a curve in the penis lumps on the side of the penis the penis becoming narrower or shorter than usual A person should see a doctor if they notice any of these symptoms. Peyronie's disease can sometimes go away without treatment. Other people with Peyronie's disease may require: oral medication medication injected into the plaque ultrasound or radiation therapy to break up the scar tissue and reduce plaque shockwave therapy, which uses electroshock waves to break up the scar tissue and reduce plaque If symptoms are severe and do not improve, a person may require surgery. Balanitis Balanitis refers to when the head of the penis becomes inflamed. This inflammation can happen in people who have not had circumcision, especially if they do not wash or dry the area underneath the foreskin properly. Other causes of balanitis can include: using strong soap or chemicals on the penis diabetes obesity Symptoms of balanitis include: a rash discharge swelling itching tenderness or pain If a person does not seek treatment for balanitis, it can cause phimosis, wherein the foreskin becomes too tight to pull back from the head of the penis. Treatment options for balanitis include: topical antibiotic, antifungal, or antiseptic ointment topical steroids a topical astringent solution Priapism Priapism causes a prolonged erection without any sexual stimulation. It can be very painful. In some cases, the cause is unknown. In other cases, however, priapism can be a result of other conditions. These conditions may include trauma to the genitals or spinal cord, sickle cell disease, or pelvic health conditions. Priapism can be a serious medical condition, and people should seek medical help if they have a prolonged, painful erection with no sexual stimulation or an erection that lasts for more than 4 hours. A person can try taking a cold shower, applying an ice pack, or climbing stairs to relieve the erection at first. Medical treatment may include: pain medications, such as opiates injecting medication into the penis to allow normal blood circulation creating a small hole or passage, called a shunt, to allow normal blood flow between the penis and the rest of the body Sexually transmitted infections People may experience pain in the penis due to a sexually transmitted infection (STI). Symptoms of an STI can include: painful ejaculation yellow, white, or clear discharge lumps around genitals pain or a burning sensation when urinating pain during sex a rash or itchiness Treatment for STIs can include: antibiotics for bacterial STIs, such as chlamydia, gonorrhea, and syphilis medications to treat symptoms of viral STIs, such as herpes Urinary tract infections If bacteria enter the urinary tract, it can cause a urinary tract infection (UTI). They are more common in females, but they can also affect males. Generally, these infections are quite common. In addition to penis pain, symptoms of a UTI in males may include: pain or a burning sensation when urinating feeling the need to urinate when bladder is empty a frequent urge to urinate blood in the urine A doctor will usually prescribe antibiotics to treat a UTI. Prostatitis Prostatitis is inflammation of the prostate, which can cause pain in the penis and pelvic area. Bacterial infections, nerve inflammation, and injuries can all cause prostatitis. Symptoms of prostatitis include: difficulty urinating pain or burning when urinating pain in the penis, testicles, or bladder painful ejaculation People can take antibiotics to treat prostatitis. Pain relief medication, prostate massage, and hot compresses can also help ease symptoms. Urethritis Urethritis is inflammation of the urethra, which is the tube that carries urine from the bladder through the penis. Causes of urethritis include: bacteria viruses injury reaction to spermicides or contraceptive lotions Symptoms may include: an itchy, tender, or swollen penis a frequent urge to urinate burning sensation when urinating small bumps in the groin area pain during sex or ejaculation A doctor will usually prescribe antibiotics to treat urethritis. Phimosis Phimosis occurs when the foreskin tightens so much that it is too tight to pull back. It is common in young children before the foreskin loosens, but it can also cause painful symptoms in teenagers and adults. Treatment for phimosis usually includes applying a steroid cream to the foreskin daily. Taking pain relievers may also help. Paraphimosis Paraphimosis is a condition in which people are unable to pull the foreskin forward over the tip of the penis. Paraphimosis is a serious condition that requires immediate medical attention. Additional symptoms include: pain in the penis swelling in the tip of the penis the head of the penis turning a different color, such as blue or red Treatment for paraphimosis involves reducing the swelling at the tip of the penis to allow the foreskin to return to the correct position. If doctors are unable to do this, they may make a small incision to reduce the swelling. In some cases, people may need a circumcision. Penile fracture A penile fracture occurs when an erect penis is bent, causing a part of it to tear. It is not technically a fracture, as there are no bones in the penis. Penile fractures are most likely to happen during sex. Symptoms of a penile fracture include: a popping sound sudden loss of erection bruising and swelling of the penis bleeding from the penis blood in the urine pain difficulty urinating Anyone with a penile fracture needs emergency medical attention. They may need surgery to drain a buildup of blood and repair any damage to the penis. Penile cancer Pain in the penis can sometimes be a symptom of penile cancer, although is more likely to be a result of another condition. People should see their doctor if they notice any of the following symptoms: changes to the color or thickness of the skin of the penis a lump or crusty bumps on the penis bleeding ulcers bleeding or discharge under the foreskin swelling at the head of the penis lumps under the skin in the groin area Treatment for penile cancer may include: surgery to remove tumors in the penis circumcision to remove the foreskin radiation therapy to destroy cancer cells chemotherapy Summary Many different conditions can cause pain in the penis. A doctor can help identify the cause of the pain by discussing a person's other symptoms. People may be able to lower their risk of developing a penile health condition by: maintaining a healthy lifestyle keeping good personal hygiene using a condom during sex If a person experiences persistent or severe penis pain, they should speak to a doctor. |
|
#213
|
||||
|
||||
|
Re: Sexual Health News
What to do about dry skin on the penis
By Lana Burgess https://www.medicalnewstoday.com/articles/325286.php The skin on a person's penis is particularly sensitive, and dry skin may cause discomfort. A person may develop dry skin on their penis skin for many reasons, including unlubricated sex or masturbation, chafing clothes, and use of harsh soaps. Dry skin on the penis by itself is not usually a sign of a sexually transmitted disease. Most cases of dry skin on the penis respond well to treatment. Home remedies, such as using a natural moisturizer or avoiding harsh soaps, often resolve the problem. This article explores what causes dry skin on the penis. It also discusses treatment for each cause and the home remedies that might help. Unlubricated sex or masturbation Having sex or masturbating for a long time without lubrication can cause friction. Too much friction may cause the skin to become dry. Using lubricant may increase comfort when a person has sex or masturbates. A range of lubricants is available online. Avoid lubricants with ingredients such as glycerin or parabens as they may worsen penis skin dryness. Choosing a water-based lubricant will reduce the chance of further penis skin irritation. Allergy to latex If a person is allergic to latex, using latex condoms may lead to dry skin on the penis. Latex is a natural substance that derives from the sap of rubber trees. People with a latex allergy react to specific proteins that latex contains. The symptoms of an allergic reaction to latex include: hives itching stuffy or runny nose wheezing chest tightness difficulty breathing People with a severe latex allergy may experience anaphylactic shock when they come into contact with latex. If a person goes into anaphylactic shock, call emergency services. If the person has an epinephrine (adrenaline) auto-injector, administer this. To avoid dry skin on the penis and allergy symptoms, people with latex allergies should use non-latex condoms. Non-latex condoms contain polyurethane or natural membranes that come from lamb's intestines. There are many non-latex condoms available to buy online. Chafing clothes If a person's clothes or underwear are too tight, they may chafe the penis and lead to dry skin. Wearing loose or cotton underwear and clothes will also help to avoid further chafing. To bring relief to chafed skin, use a natural moisturizer, such as coconut oil. Personal soaps Using soaps that contain harsh chemicals may cause dry skin on the penis. The best way to wash the penis is with warm water and a small amount of mild soap. If a person does want to use regular soap in this area, they may want to consider using a gentle, natural soap without parabens. Many soaps with no parabens are available to buy online. Laundry detergents Certain laundry detergents that contain harsh chemicals may cause skin dryness. This may affect a person anywhere on their body, including their penis. Choosing natural, non-biological laundry detergents may reduce skin irritation and dryness. To relieve irritated skin, using a natural moisturizer, such as coconut oil, may help. Eczema If dry skin on the penis occurs alongside itching or under-skin bumps, it may be a sign of eczema. An irritant, such as those explored above, can cause eczema. Doctors call this type of eczema irritant contact dermatitis. The two other types of eczema that may lead to dry skin on the penis are atopic eczema and seborrheic dermatitis. If a person thinks eczema has caused the dry skin on their penis, they should see their doctor. The doctor can diagnose or rule out eczema. People who already have an eczema diagnosis may use a low-strength topical corticosteroid cream. Applying this carefully to the penis skin may improve symptoms. It is essential to use corticosteroid creams according to a doctor's recommendations as they may increase skin thinness. As the skin on the penis is delicate and sensitive, people should take extra care when using topical treatments. To reduce dryness, a person may want to use a natural moisturizer, such as coconut oil. Psoriasis Psoriasis is another possible cause of dry skin on the penis. Psoriasis is an inflammatory skin condition that frequently affects male genitalia. Psoriasis patches on the penis are not as scaly as those on other parts of the body. They may look like well-defined, thin white plaques without scales, or they may have a red ring around them. If a person spots the signs of psoriasis on their penis, they should see their doctor. The doctor can diagnose or rule out psoriasis. People who already have a psoriasis diagnosis and have plaques on their penis may be able to treat it using the same corticosteroid cream they use on other parts of their body. The doctor may recommend a medium to high-potency corticosteroid to use in intervals. This means applying the cream for 4 days, then having a 3-day break before reapplying. Another psoriasis treatment option for the penis is topical vitamin D ointment twice daily. Should psoriasis plaques on the penis remain after treatment, it is important to go back to the doctor. The doctor can rule out anything more serious. Fungal infection If a person also has a rash, swelling, or discharge, dry skin on the penis, this may be a sign of a fungal infection. Two forms of fungal infection affect the penis jock itch and balanitis. Jock itch causes a red rash. It spreads over the inner thighs from the penis. The area around the anus and buttocks may also have a rash. Balanitis is inflammation of the tip of the penis. If a person has balanitis, the head of their penis may appear red and swollen. A yeast infection is a common cause of infectious balanitis. Both jock itch and balanitis may occur alongside itchy skin. A person with a yeast infection may feel fatigued, although studies are yet to confirm this as a symptom. People can treat fungal infections with antifungal creams. To prevent them, a person should wash and change their clothes frequently. Wearing loose underwear may also help. Home remedies Depending on the cause of the dry skin, a person may need to use over-the-counter (OTC) or prescribed topical treatments. Some home remedies may have complementary uses alongside other treatment. A doctor can provide a person with recommendations on which treatments and home remedies will suit them best. It is wise to avoid having sex or masturbating until the dry skin has started to heal. Having sex may irritate the penis skin further and slow down the healing process. Proper hydration is a good way to ensure that the skin gets enough moisture from within. Using natural moisturizers may also reduce dryness. Coconut oil offers a natural way to reduce skin dryness all over the body, including the penis. People can also use it as a massage oil or natural lubricant. Results of a 2014 study suggest that applying coconut oil may be a more effective atopic dermatitis treatment than mineral oil. Many coconut oil moisturizers are available to buy online. However, it is important to note that oils may reduce the effectiveness of condoms. Prevention To prevent dry skin on the penis, it is a good idea to: use natural, non-biological washing detergents avoid using harsh personal soaps wash the penis regularly with warm water and only a small amount of mild soap wear cotton clothing and supportive, but not overly tight, underwear use lubrication to reduce friction during partnered or solo sex keep the skin moisturized Summary Dry skin on the penis is not typically a sign of a serious condition. Common causes are allergies to chemicals in soap or detergent, too much friction, psoriasis, or eczema. If a person experiences dry skin on the penis and does not know the cause, they should see their doctor. It is particularly important to see a doctor if dry skin on the penis occurs alongside other symptoms. Typically, people can treat dry skin on the penis either at home or with OTC topical treatments. Using a natural moisturizer, such as coconut oil, is a simple way to maintain skin health. Making lifestyle changes may help to prevent dry patches on the penis from coming back. For example, a person can try reducing the use of personal soaps, changing washing detergent, and using lubricant during sex or masturbation. |
|
#214
|
||||
|
||||
|
Re: Sexual Health News
What to know about genital warts in women
By Beth Sissons https://www.medicalnewstoday.com/articles/324679.php Genital warts are a very common sexually transmitted infection. They can develop on or around the genitals and may appear as small bumps or fleshy growths. These warts result from infection with the human papillomavirus (HPV). People who have the virus can pass it on through vaginal, anal, or oral sex. Genital warts can cause discomfort, but they do not lead to other health problems and are not cancerous. A doctor can prescribe treatments for relieving symptoms, and they can also remove the warts. In this article, we investigate the symptoms, causes, and risk factors of genital warts in the female body. We also describe diagnosis, treatment, complications, and prevention. Symptoms Anyone can get genital warts. In females, genital warts can develop in or around the: vagina vulva cervix anus groin region and upper thighs Because the virus can spread through oral sex, warts can also appear on the lips, mouth, and throat. Genital warts tend to look like small, fleshy bumps or growths. The number of warts can vary, and clusters may develop in a formation that resembles a cauliflower. Genital warts are usually the same color as the person's skin or slightly darker. The bumps may be smooth or rough. Also, they can be too small to notice. Often, genital warts do not cause symptoms. However, they can occur with: itching burning tenderness or pain bleeding 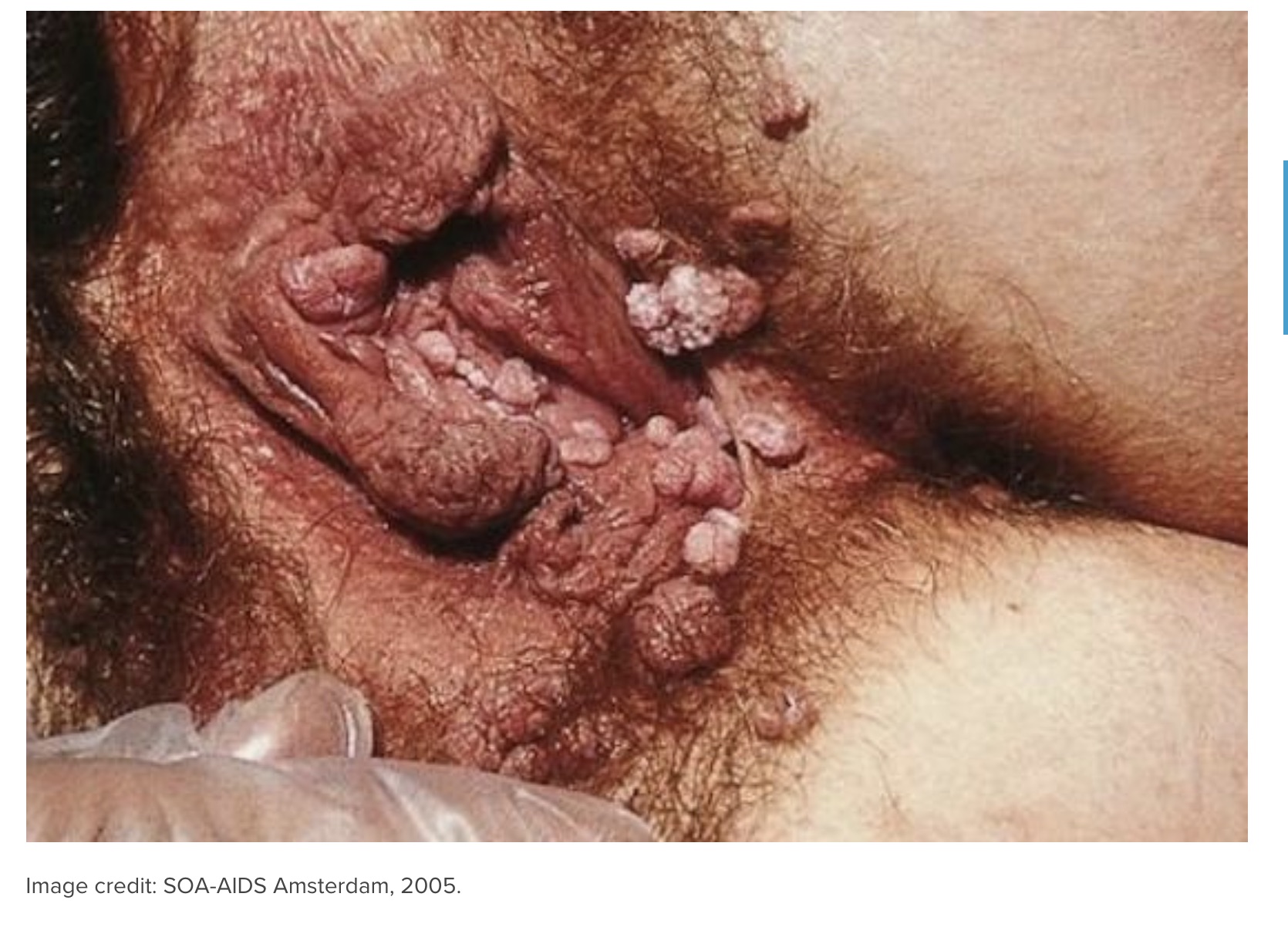  Causes Genital warts result from infection with HPV. This is a type of sexually transmitted infection (STI). According to the Centers for Disease Control and Prevention (CDC), HPV is the most common STI in the United States. It affects around 79 million people in the country, mostly adults under the age of 30. There are around 14 million new HPV infections each year in the U.S. A person with an HPV infection can pass on the virus through: vaginal, anal, and oral sex skin-to-skin genital contact childbirth Genital warts do not always appear immediately after a person becomes infected they can take months or even years to develop. The CDC note that most people fight off the virus without treatment and that, in this case, it does not cause any health problems. Once the virus goes, a person can no longer pass it on. There are many different types of HPV. The type of HPV that causes genital warts does not cause cancer. Risk factors Anyone who is sexually active is at risk of an HPV infection. Other risk factors include: smoking having a weakened immune system being under the age of 30 When to see a doctor When a person notices that they have genital warts, they should see a healthcare professional, for example at a sexual health clinic. Sometimes genital warts clear up on their own over time. However, getting treatment can reduce the risk of transmission and help ease uncomfortable symptoms, such as itching and pain. Diagnosis Healthcare professionals usually diagnose genital warts with a physical examination. To see the warts better, they may use a colposcope or apply a vinegar solution to the genital area, if the warts are not visible to the naked eye. A healthcare professional may also take a small sample of a visible wart and send it for analysis. This testing can help confirm the diagnosis. Treatment There is currently no treatment for HPV. A person's immune system often fights off the virus over time. If genital warts are causing discomfort or distress, a doctor can prescribe treatments to relieve symptoms or remove the warts. This treatment can also help reduce the risk of passing on the infection to other people. Topical treatments for genital warts include: podofilox imiquimod podophyllin trichloroacetic acid For people with larger or more difficult-to-treat warts, the doctor may recommend removing them. The following are some removal methods: Cryotherapy. This involves freezing off the warts with liquid nitrogen. Cryotherapy may cause a burning sensation, as well as pain and blistering. Surgical excision. This involves a doctor cutting away the warts. Before the procedure, they will give the person a local anesthetic to numb the area. Electrocautery. This involves a doctor burning the warts off the skin with an electrical device. A person may require a local or general anesthetic. Laser therapy. In this procedure, a surgeon uses a powerful beam of light to destroy the warts. It can cause pain and irritation afterward. It is important not to use treatments for other types of warts on genital warts. Doing so can make symptoms worse. Removing genital warts does not get rid of the HPV infection. They may return after treatment and a person can still pass on the virus. Also, wearing a condom during sex can help lower the risk of transmission but does not completely prevent it. Complications There are over 100 different types of HPV. The types that cause genital warts do not cause cancer. Even if a person does not receive treatment for their genital warts, the warts will not become cancerous. However, a person can have more than one type of HPV infection at a time, and at least 14 types can cause cancer, including cervical cancer. When a female has genital warts, a doctor may suggest screening for signs of cervical cancer or high-risk types of HPV. The U.S. Preventive Services Task Force recommend that all females: aged 2129 years have a cervical screening, also known as a Pap smear or smear test, every 3 years aged 3065 years have a Pap smear every 3 years, or a Pap smear plus an HPV test every 5 years Females aged 30-65 years also have the option of just having an HPV test every 5 years. If a Pap smear gives an unclear or abnormal result, it does not mean that a person has cancer. The doctor will carry out additional tests to look for any changes in the cells of the cervix. Pregnant women with a past history of genital warts should inform their healthcare providers. This is unlikely to cause any pregnancy complications or affect the baby. Also, having genital warts during pregnancy can make the delivery more difficult. Prevention Wearing a condom during sex lowers the risk of getting genital warts. However, a condom does not cover the whole genital area and so may not completely protect against HPV transmission. Other methods of birth control do not protect against genital warts. It is important for people to tell their sexual partners if they have these warts. Getting an HPV vaccination can also help protect against the types of the virus that can cause genital warts or cervical cancer. The CDC recommend HPV vaccination for all children at 11 or 12 years of age and for all females aged 1326 years. According to the Office on Women's Health, the Food and Drug Administration (FDA) have approved the HPV vaccine for people aged 945 years. Anyone with any severe allergies or an allergy to yeast should consult their doctor before getting the vaccine. The CDC do not recommend the HPV vaccine for women who are pregnant. Stopping smoking can also lower the risk of getting genital warts. Summary Infection with some types of HPV can cause genital warts. These can form in or around the vulva, vagina, or cervix. The warts may appear on their own or in cauliflower-like clusters. They can cause itching, tenderness, or a burning sensation. Genital warts are generally harmless and are not cancerous. The types of HPV that cause genital warts do not cause cervical cancer. Although there is no treatment for the virus, a doctor can prescribe medications to relieve symptoms. They can also remove the warts. For large or difficult-to-treat warts, a doctor may recommend surgical removal. A person can pass on HPV through vaginal, anal, or oral sex. Wearing a condom during sex can help reduce the risk of getting and spreading genital warts. HPV vaccination can also protect against genital warts and cervical cancer. |
|
#215
|
||||
|
||||
|
Re: Sexual Health News
Is the shot or the pill better for birth control?
By Rachel Nall MSN CRNA https://www.medicalnewstoday.com/articles/324716.php The shot and the pill are two effective forms of hormonal birth control, each with their own benefits and risks. Does one work better than the other? There are many different birth control options. People can choose which one to use based on their benefits, risks, and what feels right. When choosing between the shot and pills, people may want to consider their effectiveness, side effects, risks, and convenience. This article will discuss the benefits and risks of the shot and pills for birth control, and tips for how to choose between them. What are birth control shots and pills? Hormonal birth control comes in several forms, including an injectable shot and oral pills. A person needs to take birth control pills at the same time each day. When using the shot, a person will receive injections of a hormone every 3 months. There are many different brands of birth control pills, each with slightly different levels of hormones. There are two main groups of pills: combination contraceptive pills that contain estrogen and progestin progestin-only pills, or mini-pills The birth control shot, or Depo-Provera, also contains progestin, which is the hormone that prevents ovulation. Progestin, which all pills and shots use, prevents the ovaries from releasing an egg. This makes pregnancy very unlikely. The hormone can also make the lining of the uterus less favorable for an egg to implant. The estrogen component in the combination pills actually thickens the uterine lining, which provides stability and controlled bleeding patterns. This is why people taking the combination pill usually have a regular monthly period. Effectiveness According to the Office on Women's Health, the effectiveness rates of the shot and the pill are slightly different: About 6 out of every 100 women who have the shot will become pregnant within the first year. About 9 out of every 100 women who take the pill will become pregnant within the first year. If someone does not get the shot as regularly as every 3 months, they have a greater likelihood of becoming pregnant. Likewise, if a person misses a pill or takes it later than the ideal time, this could make the pill less effective. Certain medicines can interfere with both the birth control shot and pills, which could reduce their effectiveness. A person should ask their doctor about drug interactions when taking a new medicine, including antibiotics. If someone wants to become pregnant after stopping birth control injections, it takes 10 months, on average. Side effects As with most medications, birth control pills and the shot have side effects. People may wish to discuss these with their doctor when considering the best option for them. The side effects are similar for the shot and pills because they contain similar hormones. Side effects for the birth control shot include: bleeding between periods bone loss when a person uses this option long-term headaches missed periods mood changes sore breasts weight gain Doctors may advise that a person receiving birth control shots take calcium supplements to reduce the risk of bone loss. When they stop receiving birth control injections, they will usually gain lost bone back. Side effects for birth control pills include: headache increased blood pressure mood changes sore breasts stomach upset weight gain Doctors associate the mini-pill with fewer side effects than combination contraceptives. In rare cases, taking the combination pill can cause blood clots and a higher risk of heart attack and stroke. People are more likely to experience these complications if they are older than 35, if they smoke, or if they have a history of migraine. Bleeding patterns With the shot, people may experience more sporadic bleeding patterns, but as time goes on, they tend to have much lighter, less frequent episodes of bleeding. Some people even have total absence of periods after a while. The one drawback is that they will not necessarily know when they are going to bleed. With pills, people may have irregular bleeding initially, but generally, this will become a regular predictable bleed each month. People can also take pills on an extended cycle to avoid having periods every month. For the most part, they will know when to expect a period. However, if they miss pills, they may bleed unexpectedly. Cost The cost of birth control varies depending on manufacturers and types. Health insurance companies and family planning clinics often cover or discount the costs of birth control pills and shots. According to the National Women's Health Network, one birth control shot costs $60. Birth control pills typically cost up to $50 per month, but generic forms of pills can cost as low as $10 per month. Which one is right for me? When a person uses them as a healthcare professional directs, birth control pills and the shot can both effectively prevent pregnancy. Some of the major considerations include: Convenience. If someone is worried that they will not be able to take their pills at the same time every day, they may prefer the shot. If they do not want to go back to the doctor's office every 3 months, birth control pills may be more convenient. Bleeding patterns. Both the shot and pills can cause changes in menstruation. The shot can make periods lighter, less frequent, and unpredictable for some people. Combination pills can help regulate a person's menstrual cycle and allow them to predict when their period arrives. Effectiveness. Both contraceptive methods have similar effectiveness when a person uses them appropriately, though the shot may be slightly more effective than the pill. Side effects. Both methods have side effects. Some people may have different side effects than others, as each person's body reacts differently to hormones. Cost. The cost of the pills and the shot can be similar depending on a range of factors, such as brands, a person's insurance, and whether they are able to get the birth control from a family planning clinic. Alternative birth control options Aside from the shot and pills, people can use other prescription or nonprescription methods of preventing pregnancy. Nonprescription birth control options include: female condoms male condoms spermicides sponges Prescription methods include: diaphragms implantable rods intrauterine devices patches vaginal rings People can use a prescription or nonprescription method together with male or female condoms for protection against sexually transmitted infections (STIs). Sponges and spermicide may not prevent STIs. Summary Birth control pills and the birth control shot are both effective ways to prevent pregnancy. Both use similar hormones, so they also have similar side effects and risks. Some people prefer the convenience of only having to get a birth control injection every 3 months, while others may not like having to make extra appointments with their doctor. Ultimately, a person should consider many factors when determining what option may work best for them. |
|
#216
|
||||
|
||||
|
Re: Sexual Health News
What causes watery semen, and does it affect fertility?
By Jamie Eske https://www.medicalnewstoday.com/articles/325058.php Semen is typically a thick, white fluid, but it can vary in color and consistency. Watery semen can occur due to low sperm count, lifestyle factors, and nutritional deficiencies. In this article, we explore some of the possible causes of watery or clear semen. We also discuss whether watery semen can affect fertility, the meaning of discolored semen, when to see a doctor, and treatment. Low sperm count The World Health Organization (WHO) define low sperm count, or oligospermia, as producing fewer than 15 million sperm per milliliter of semen. Having a low sperm count can make it more difficult for a person to conceive but does not necessarily mean that a person is infertile. There is not always an obvious cause for having a low sperm count. However, some genetic conditions, such as Klinefelter syndrome, can affect a person's sperm count. Other causes of low sperm count can include: hormone disorders, such as hyperthyroidism and hypogonadism infections exposure to radiation or toxins, such as industrial chemicals, herbicides, and lead drug use excessive alcohol intake tobacco use excess body weight certain medications Varicocele A varicocele is a swelling of the veins that run from the testicles to the scrotum. Varicoceles may not cause symptoms, but they can reduce sperm production and decrease semen quality in some people. Varicoceles can develop in one or both sides. Varicoceles are very common. According to the Urology Care Foundation, varicoceles affect around 15% of males, and around 40% of males tested for fertility issues have this condition. That said, around 80% of people with a varicocele do not have any fertility issues. Frequent ejaculation Frequent ejaculation may lead to watery semen. If a person masturbates or engages in sexual activity multiple times per day, their body may not have enough time to produce the same volume or quality of semen. In a 2016 study, 20 males followed a daily ejaculation schedule for 14 days after 35 days of abstinence. The researchers collected and analyzed the participants' semen samples on days 1, 3, and 14 of the study. They found that both the semen volume and the amount of available sperm decreased between days 1 and 3 and again between days 7 and 14. Retrograde ejaculation During ejaculation, semen passes through the urethra and out of the penis. However, a dysfunctional bladder sphincter can cause semen to travel backward into the bladder, resulting in a condition called retrograde ejaculation. People who experience retrograde ejaculation may produce less semen or semen that appears thin or watery. Zinc deficiency Zinc is an important nutrient that supports many essential bodily functions, such as DNA synthesis, fighting off infections, wound healing, and reproduction. Zinc also plays a role in healthy sperm production. According to a 2018 review article in the Journal of Reproduction and Infertility, zinc deficiency may contribute to poor semen quality and infertility. However, the authors caution that too much zinc can also reduce sperm quality. The body cannot produce or store zinc, which means that people can only get zinc from the foods they eat. Some dietary sources of zinc include: oysters red meat, poultry, and shellfish nuts, seeds, and whole grains beans yogurt and other dairy products Can watery semen affect fertility? Watery semen is often temporary and may resolve on its own. Persistent watery semen can sometimes indicate a low sperm count or another condition that may affect fertility. Having a low sperm count does not necessarily mean that a person is infertile, but it can make it more difficult to conceive. Watery semen can also be due to lifestyle factors, nutrient deficiencies, or an underlying medical condition. According to the National Institute of Child Health and Human Development, most male fertility problems occur due to issues affecting how the testicles work. What does it mean to have discolored semen? Discolored semen can sometimes indicate a health problem. Pink, red, or brown semen may contain blood from an inflamed prostate or swollen seminal vesicles. Other causes of blood in the semen include: high blood pressure sexually transmitted infections a prostate infection cancer of the prostate, testicles, or urethra Yellow semen may contain urine or an excessive amount of white blood cells. The latter occurs in a condition called leukocytospermia. Green semen can indicate an infection of the prostate or other reproductive organs. When to see a doctor People with persistent watery or discolored semen should speak with a doctor or urologist. Also, a person should seek medical advice for watery or discolored semen that occurs with any of the following symptoms: unusual discharge difficult or painful urination pain or discomfort in the testicles or scrotum pain in the lower abdomen or lower back fever chills nausea People who wish to conceive may want to consider consulting a fertility specialist if they have not achieved pregnancy after 1 year of having regular unprotected intercourse. To diagnose the cause of watery or discolored semen, a doctor will ask a person about their symptoms, medical history, and lifestyle habits. If necessary, they may also perform a physical examination. The doctor may also request a semen sample, which they will analyze for: volume and consistency acidity sperm count sperm motility, or how quickly the sperm move the size and shape of the sperm Treatment Treatment options for watery or discolored semen will depend on the underlying cause. A doctor may prescribe antibiotics if they determine the cause to be a bacterial infection. For people with hormonal imbalances, a doctor may recommend hormone therapy. Options for treating varicoceles include: Laparoscopic surgery. During this procedure, a surgeon inserts a camera into a small incision in the abdomen. They will then locate and either repair, block, or remove the varicocele. Percutaneous embolization. This is a minimally invasive procedure in which a surgeon will insert a coil or balloon into the swollen vein. They then enlarge the coil or balloon to restore the blood flow from the testicle. Lifestyle changes that can help improve semen quality can include: maintaining a healthy body weight reducing stress getting enough sleep quitting tobacco products reducing alcohol intake Summary Watery semen is often temporary, and it may resolve on its own. Semen can become watery or thinner than usual if someone masturbates or engages in sexual activity multiple times each day. In this case, abstaining from sexual activity for a few days may help treat the issue. Watery semen can sometimes indicate that a person has a low sperm count or reduced semen quality. These can result from certain medical conditions and lifestyle factors. Having watery semen does not necessarily mean that a person is infertile. However, people with persistent watery semen may wish to consult a doctor. Also, seek medical advice for discolored semen or semen that contains blood. |
|
#217
|
||||
|
||||
|
Re: Sexual Health News
What to know about urethral syndrome
By Amanda Barrell https://www.medicalnewstoday.com/articles/325057.php Urethral syndrome describes a group of symptoms that occur when the urethra becomes irritated. The urethra is the tube that carries urine from the bladder to the outside of the body. In this article, we discuss what urethral syndrome is along with its risk factors and symptoms. We also cover diagnosis, treatment, and prevention. What is urethral syndrome? Urethral syndrome, also known as urethral pain syndrome, is the term for a group of symptoms that can occur when the urethra becomes irritated. The urethra is the thin tube of muscle that runs between the bladder and the outside of the body. In males, the urethra also carries semen from the testicles during ejaculation. When the urethra becomes irritated, it swells up and the tube narrows, which can make it more difficult for a person to pass urine. The symptoms of urethral syndrome are similar to those of urinary tract infections (UTIs) and urethritis, which can also affect the urethra. However, bacterial and viral infections are not the cause of urethral syndrome. Urethral syndrome can occur in both males and females. Symptoms The symptoms of urethral syndrome can include: needing to urinate more often than usual pain during urination sudden urges to urinate the bladder not feeling empty after urinating discomfort or pain in the abdomen pain in the lower back pain in the genitals pain during sex Males with urethral syndrome may also experience discharge from their penis and symptoms relating to sexual function, such as swollen testicles, pain while ejaculating, and blood in the semen. Risk factors Doctors do not fully understand what causes urethral syndrome. However, certain health conditions and environmental factors can increase a person's risk of developing urethral syndrome. Some possible risk factors of urethral syndrome include the following: Sexually transmitted infections Sexually transmitted infections (STI) can increase the risk of developing urethral syndrome. STIs that may lead to urethral syndrome include gonorrhea, chlamydia, and mycoplasma genitalium. Foods Substances in certain foods can enter the urine and irritate the urethra. Foods that may increase the risk of urethral syndrome in some people include: foods and beverages containing caffeine hot or spicy foods alcohol Irritants Chemicals in soaps, personal hygiene products, and contraceptives can contain chemicals that irritate the urethra in some people. These can include: scented soaps, body washes, and bubble baths feminine hygiene sprays or douches sanitary products contraceptive gels condoms Urinary tract infection People can sometimes develop urethral syndrome after recently having a UTI. This is because the urethra can be very sensitive while recovering from an infection. Sexual intercourse Rough sexual activity can damage the urethra, especially in females. In these instances, the inflammation that leads to urethral syndrome is part of the natural healing process. Other risk factors Other risk factors for urethral syndrome can include: having sex without a condom having a history of STIs bacterial infections in the bladder or kidneys taking medications that suppress the immune system structural problems, such as a narrow urethra Women who have given birth to several children may also be at greater risk of urethral syndrome. Having a delivery without an episiotomy, which is when a doctor makes an incision in the tissue between the vagina and the anus, can also increase a woman's risk of developing urethral syndrome. Diagnosis A doctor, who is usually a specialist called a urologist or a urogynecologist, will diagnose urethral syndrome. Diagnosis can be difficult because the symptoms are often similar to those of other conditions, such as UTI, urethritis, or cystitis. Urologists usually only diagnose a person with urethral syndrome after ruling out other possible causes. In most cases, the urologist will request a urine sample. They will also ask the person about their symptoms, risk factors, and medical history. The urologist may also carry out a physical examination. Treatment Treatment depends on the suspected cause of the condition. For people with an STI, UTI, or other infection, a urologist may prescribe medications to treat the infection. They may recommend a course of antibiotics if the infection is bacterial. A urologist may also prescribe medications to relieve pain and inflammation. If the urologist suspects that the cause is an irritating soap or hygiene product, then they may recommend the person tries stopping or changing products. Further treatment may not be necessary. Some urologists also recommend making dietary changes to help treat urethral syndrome. In a 2002 study, researchers asked females with urethral syndrome to follow a strict diet for 12 weeks that did not allow any coffee, alcohol, or spicy foods. Of the 675 women who took part, 89 percent reported that their symptoms had completely gone by the end of the trial. Prevention It may not always be possible to prevent urethral syndrome. However, a person can reduce their risk of developing this condition by: using a condom during sex using perfume-free body washes, bubble baths, and sanitary products limiting or reducing alcohol and caffeine intake avoiding hot or spicy foods Summary Urethral syndrome refers to a group of symptoms that affect the urethra, which is the thin tube of muscle which connects the bladder to the outside of the body. These symptoms can include urination difficulties and pain or discomfort in the lower abdomen. Doctors do not fully understand what causes urethral syndrome. However, risk factors for urethral syndrome can include infections and irritants from certain foods and hygiene products. Treatment of urethral syndrome often involves treatment of any underlying conditions or avoiding foods and hygiene products that can irritate the urethra. |
|
#218
|
||||
|
||||
|
Re: Sexual Health News
Causes and treatment of vaginal cuts
By Jennifer Huizen https://www.medicalnewstoday.com/articles/325100.php Minor vaginal cuts and tears are common and often occur when a person is removing body hair or engaging in sexual activity. People with certain hormonal, skin, and immune conditions may be more likely to get vaginal cuts or tears. Minor vaginal wounds are usually harmless, but they may cause mild pain and discomfort for a day or two before they heal, particularly during urination and bathing or showering. Some minor cuts or tears may also bleed lightly for a short period. More severe cuts or tears can require medical attention, especially those that are deep, will not stop bleeding, or do not heal with proper self-care. In this article, we discuss some common causes of vaginal cuts and tears. We also cover treatment, prevention, and when to see a doctor. Sexual activity Sexual activity is a common cause of vaginal tears. A penis, finger, or another object that a person inserts into the vagina can damage its delicate tissues. Following sexual activity that causes vaginal tears, a person may also have minor bruising in the pelvic region and vaginal soreness that lasts for a few days. Factors that may increase the likelihood of vaginal tears during sexual activity include: rough or vigorous thrusting of an object into the vagina vaginal dryness vulvovaginal atrophy, a condition in which the vaginal tissues become drier, thinner, and less elastic vaginal scarring or tissue damage, for example, from surgery, pelvic radiation therapy, or congenital abnormalities certain skin conditions, such as eczema, lichen planus, or psoriasis some medications, including corticosteroids Hair removal Removing pubic hair with a razor is another common cause of vaginal cuts or tears. Waxing can also cause noticeable skin tears or cuts. According to a 2017 study, about 25% of people injure themselves while grooming their pubic hair. Individuals with skin conditions may be more prone to cuts and wounds during hair removal. In addition to larger cuts or tears, all forms of hair removal can cause microscopic wounds. These tiny wounds are still large enough to allow germs to enter the body so they may increase the risk of skin infection. Vaginal delivery Vaginal delivery can cause more severe cuts or tears inside the vagina. According to the American College of Obstetricians and Gynecologists, 5379% of women who deliver vaginally develop lacerations, or cuts. Cuts or tears from vaginal deliveries can be painful and may make it difficult for a woman to walk or sit for a few days. More severe cuts or tears can be very painful and may bleed. The perineum, which is the space between a person's anus and vulva, is also typically swollen and sore for a few weeks. Treatment Cuts and tears compromise the skin barrier, which makes it easier for germs to enter the body and cause an infection. Keeping the area around a vaginal cut clean and dry can help prevent skin infections. Some general suggestions for treating vaginal cuts and tears include: washing the hands with soap and running water for 1530 seconds before touching the wound washing the affected area daily with warm water and a mild, unscented soap or cleanser making sure that the affected area is completely dry before getting dressed avoiding soaking the affected area taking over-the-counter pain relievers to reduce discomfort applying a covered ice pack to the area to reduce inflammation and discomfort using a peri bottle during and after urination to minimize pain avoiding getting any paper towel in the wound using a pillow if sitting is uncomfortable applying witch hazel to a sanitary napkin to reduce discomfort avoiding using products inside the vagina avoiding harsh or scented products that can interfere with the acidic pH of the vagina While vaginal cuts or tears are healing, a person may wish to avoid sexual activities that involve the vagina. Wearing loose-fitting underwear made of natural materials, such as cotton or bamboo, for a few days may also help. Prevention It is not always possible to prevent vaginal cuts and tears. However, depending on the cause, a person can take some steps to reduce the risk of vaginal wounds. Sexual activity Ways to lower the risk of vaginal cuts and tears during sex include: using a water- or silicone-based lubricant setting aside time for sex to ensure that no participant is anxious, rushed, or too tired making time for foreplay and arousal telling a sexual partner about pain and stopping if the pain becomes too severe emptying the bladder before sex having a warm bath before sex to relax the vaginal muscles People using condoms should not use mineral oil, baby oil, or petroleum jelly as a sexual lubricant because these products can damage latex. Regular vaginal intercourse helps keep the vaginal tissues elastic and strong, which can make vaginal cuts and tears less likely. Hair removal To prevent cuts and injuries while trimming or shaving pubic hair, the American Academy of Dermatology suggest: avoiding distractions and not letting the mind wander while shaving wetting the skin and hair before shaving using shaving creams or gels using a clean razor with a sharp blade rinsing the razor clean after each stroke shaving in the direction of hair growth standing up while trimming or shaving and avoiding lying down trimming or shaving oneself as someone else cannot feel what is happening storing razors in a cool, dry place throwing away disposable razors after five to seven uses being extra cautious and shaving lightly when going over acne sores or scars The following tips can help prevent vaginal tears while waxing: making sure that the area is clean, dry, and free of any irritation, wound, or sore applying the wax in the direction of hair growth and removing it in the opposite direction keeping the skin taut when applying and removing the wax Vaginal delivery Cuts or tears are a fairly inevitable consequence of vaginal delivery. However, healthcare professionals may use certain techniques to help prevent these injuries, including: perineal massage to reduce muscular resistance, either during the second stage of labor or shortly after delivery applying warm compresses to the perineal area while a woman pushes during labor Doctors are also reconsidering the safety and effectiveness of episiotomy, which is a procedure that involves making a deep cut during delivery to enlarge the woman's birth canal. When to see a doctor Minor vaginal cuts or tears are generally harmless and usually heal quickly without treatment. However, more severe cuts or tears can lead to complications, such as substantial blood loss and infections. It is important to see a doctor for vaginal cuts or tears that: bleed excessively or do not stop bleeding after 10 minutes of applying firm, direct pressure are large, deep, or numerous have rugged edges do not heal within a few days get worse cause concern or distress People with vaginal cuts or tears should seek immediate medical care if they also have any of the following symptoms: fever or chills discolored or foul-smelling discharge a general feeling of being unwell numbness or tingling feeling faint or losing consciousness People who frequently experience painful or large vaginal cuts or tears should discuss their symptoms with a doctor to identify possible underlying conditions. Sexual abuse, assault, or rape can cause vaginal cuts or tears of varying severity. People who have experienced sexual violations should talk to a doctor as soon as possible or seek emergency care. Adults should also speak with a doctor about any unexplained or concerning vaginal cuts or tears in children or infants. Summary Vaginal cuts or tears can occur during pubic hair removal and sexual activity. Vaginal delivery during childbirth can also cause wounds in the tissues inside and surrounding the vagina. Minor vaginal cuts or tears can cause pain and discomfort, but they generally heal without treatment within a few days. Keeping the affected area clean and dry can help the wounds heal and prevent infection. More significant cuts or tears may require medical attention. See a doctor if the cuts are deep, numerous, or do not stop bleeding. |
|
#219
|
||||
|
||||
|
Re: Sexual Health News
HIV-positive man who avoided taking test, possibly infecting others, gets jail
https://www.channelnewsasia.com/news...ction-11876898 SINGAPORE: An HIV-positive man who had casual sex frequently with other men was on Thursday (Sep 5) sentenced to three-and-a-half years' jail, after pleading guilty to two charges under the Infectious Diseases Act as well as three drug-related charges. The 35-year-old Malaysian started engaging in sexual activity with men in Singapore in 2003, the court heard. Although he suspected that he could have been exposed to HIV or infected with it, he decided not to get tested after 2008, as he was afraid of losing his permanent residency status in Singapore if he tested positive for HIV. According to the person who reported him to the Ministry of Health (MOH), at least six other men who had sex with him were later diagnosed with the human immunodeficiency virus, which could lead to Acquired Immune Deficiency Syndrome (AIDS). The man cannot be named due to gag orders issued by the court. He was a freelance hairdresser and fashion designer at the time of the offences. ACCUSED WAS CONTACTED BY HEALTH AUTHORITIES SEVERAL TIMES In 2010, the accused had sex with a man who later tested positive for HIV and informed him about it. MOH's National Public Health Unit (NPHU) also contacted the accused, telling him he was a sexual contact of an HIV-positive person and advised him to go for testing. The man lied to NPHU that he gets tested regularly for the virus and had been found negative in the latest test. NPHU contacted the accused at least three times in the next five years, informing him each time that he had been named as a sexual contact of someone who had tested positive for HIV. Despite this, the man did not go for any HIV tests, even though he knew that he had been exposed to a significant risk of contracting the virus. In July 2013, the accused had unprotected sex with a man he met on social networking application Grindr, without telling him about the risk of contracting AIDS or HIV infection from him. They had sex on two other occasions. After that, the other man developed a fever and was later diagnosed with HIV infection. According to this man, the accused was the first person he had had sex with after testing negative for HIV in 2011. When NPHU again asked the accused to be tested for the virus, he lied that he had tested negative for it. He continued in his ways, meeting another man for sex in February 2014. This man asked if he was HIV positive, and the accused did not answer him, instead saying that he would get tested. The accused's sex partner was diagnosed with HIV infection in August 2014. He had last tested negative in March that year, and the accused was the last person he had sex with before his diagnosis. When the sex partner told the accused about his infection and asked if he was HIV positive as well, the accused did not answer him and told him again that he would go for a test. ACCUSED AVOIDED NPHU NPHU contacted the accused in January 2015 telling him that he posed a risk to others through his unprotected sexual activities, but the accused said he was busy with work and refused to answer NPHU when it called him about five times. An informant told MOH's Surveillance and Enforcement Branch on Mar 18, 2016 that the accused had had sex with up to six partners who were diagnosed with HIV after sex with him. The accused tested positive for HIV on Feb 13, 2017, after MOH ordered him to take the test. More than a year after this, the accused was arrested for drug offences. He had smoked methamphetamine obtained from a drug dealer, saying he abused the drug to stay awake for longer hours. He was nabbed again in April this year and admitted to smoking meth or Ice on about five occasions in March. ACCUSED WAS "WILFULLY BLIND": PROSECUTION The prosecution asked for a sentence of 45 months' jail, saying there were multiple victims and that some of the drug offences took place while the accused was on bail. "The accused is not young," said Deputy Public Prosecutor Ho Lian-Yi. "He's in his 30s ... he has his own dealer, he goes to Orchard to specifically buy drugs for his own consumption." He had chosen to be "wilfully blind" to the possibility of having HIV infection and deceived NPHU, added Mr Andre Moses Tan from MOH's legal office who handled the case with Mr Ho. "The accused had denied his sexual partners their right to make an informed decision as to whether to proceed with sexual activity with him," said Mr Tan. "In fact, the accused did not even take the simple step of using protection." Defence lawyer James Ow Yong asked for 35 months' jail instead, saying his client had no previous convictions and that he was "also bearing the brunt of his offences". "HIV is, at this point in time, an incurable disease," said the lawyer. "The accused has to live with the ... impact of this disease all his life." For his offences under the Infectious Diseases Act, the accused could have been jailed for up to 10 years, fined up to S$50,000, or both. For consuming meth, he could have been jailed for up to 10 years, fined a maximum S$20,000, or both. |
|
#220
|
||||
|
||||
|
Re: Sexual Health News
How do vaginal bacteria naturally protect against chlamydia?
By Catharine Paddock Ph.D https://www.medicalnewstoday.com/articles/326052.php New research reveals, for the first time, how certain bacteria in the vagina and cervix prime cells to defend against the most common sexually transmitted infection (STI). Scientists have known for a while that the composition of microbes, or microbiome, in the vagina and cervix can influence resilience to chlamydia. Previous research had revealed, for instance, that vaginal microbiomes with a high level of certain Lactobacillus bacteria can help defend against chlamydial infection. Until the recent mBio study, however, it was not clear how the protective bacteria were exerting their influence. The researchers, from the University of Maryland School of Medicine (UMSOM) in Baltimore, were surprised to find that the protection did not come directly from the beneficial bacteria. Instead, they discovered that resilience to chlamydial infection was the result of changes that the bacteria induced in cells in the lining, or epithelium, of the vagina and cervix. The team suggests that the findings will increase understanding of the role of the microbiome in protecting against STIs. Furthering such understanding, they note, "may enable the development of novel microbiome based therapeutic strategies to protect women from infection and improve vaginal and cervical health." Need to understand resilience mechanisms Chlamydia is a common STI. It is the result of infection by the bacterium Chlamydia trachomatis, and it is easy to treat. Both males and females can get chlamydia by having vaginal, oral, or anal sex with a person who has the infection. Chlamydia, like other STIs, can facilitate the spread of HIV. If left untreated, females with chlamydia can find it difficult to conceive. In addition, pregnant women with the infection can pass chlamydia to their babies during birth. This, in turn, raises the risk of the infant developing pneumonia and a condition that causes blindness. Chlamydial infection typically has no symptoms, and when they do occur, they usually take weeks to appear. The symptoms of chlamydia include a burning sensation while urinating and abnormal discharge from the vagina or penis. A less common symptom in males is painful and swollen testicles. In 2017, the Centers for Disease Control and Prevention (CDC) recorded a total of 1,708,569 reports of chlamydial infection. "Chlamydia is a major growing health issue in the U.S.," says senior study author Jacques Ravel, a professor of microbiology and immunology at UMSOM, "and more work is needed to understand why some women are apparently naturally protected while other[s] are not." Study investigated Lactobacillus species In previous work, the researchers had demonstrated that there are five major microbiome compositions that can inhabit the vagina. It appears that in four of the vaginal microbiome types, various Lactobacillus species of bacteria dominate. The fifth type has very low levels of Lactobacillus and is more likely to coincide with a higher risk of HIV and other STIs, as well as with premature births. In the new study, the team carried out more detailed investigations of the different vaginal microbiome compositions and of their various Lactobacillus species. They used vaginal samples from women with chlamydia, together with cultures of Lactobacillus and of the epithelial cells that line the vagina and cervix. The results showed that the species L. iners, which commonly inhabits the vagina, did not help human cells defend against chlamydial infection. In contrast, L. crispatus which is another species that also commonly inhabits the vagina did seem to protect human cells against chlamydial infection. D-lactic acid protects against chlamydia The researchers eventually pinned down the reason that some Lactobacillus species appear able to protect the cells while others do not. All Lactobacillus species produce lactic acid. However, there are two variants, or isoforms, of lactic acid: the L form and the D form. Different Lactobacillus species produce different amounts of the two forms of lactic acid. For instance, L. iners almost exclusively produces the L form of lactic acid. In contrast, L. crispatus produces both L-lactic acid and D-lactic acid, but mostly the latter. The researchers discovered that it was a predominance of D-lactic acid but not L-lactic acid that protected against chlamydial infection. It appears that D-lactic acid stops C. trachomatis from entering human epithelial cells by reducing cell proliferation, which the team had shown was a necessary condition for infection. In further tests, the researchers discovered that D-lactic acid reduced human cell proliferation by downregulating the genes that drive the cell cycle. In a final set of experiments, they then showed that an "optimal microbiome" in the vagina can offer long term protection against chlamydial infection. The researchers are continuing their investigation into how to use the findings as a basis for protecting against C. trachomatis, and how to apply them to other STIs. |
|
#221
|
||||
|
||||
|
Re: Sexual Health News
Yeast infection after sex: What to know
By Jenna Fletcher https://www.medicalnewstoday.com/articles/326110.php While sexual activity does not cause a yeast infection, it can increase the risk of one developing by introducing new bacteria to the vagina. Learn more in this article. Yeast infections are particularly common in females. They are not usually serious, and people can often treat them with medications that they can purchase from a pharmacy. According to the Office on Women's Health, most women will get a yeast infection at some point in their life. Doctors do not consider yeast infections to be sexually transmitted infections (STIs). However, sexual activity may affect whether a person develops a yeast infection. Keep reading for more information about the causes and treatments for yeast infections, as well as how sexual activity can affect the risk. Causes of a yeast infection An overgrowth of microscopic Candida causes fungus yeast infections. The Candida fungus is a normal part of the vaginal environment and is harmless when kept in balance. However, under certain conditions, this fungus may grow out of control and cause a yeast infection Can sex cause a yeast infection? Sexual intercourse does not directly cause yeast infections, and doctors do not consider yeast infections to be STIs. However, some sexual activities, such as penile, toy, or finger insertion, can introduce bacteria to the vagina. The new bacteria can potentially trigger the growth of the Candida fungus, causing a yeast infection to develop. It is also possible to develop a yeast infection following oral sex. A person's mouth and saliva also introduce bacteria. Other risk factors and prevention It is not always possible to prevent yeast infections from developing. However, there are some steps a person can take to reduce their risk factors, including: frequently changing tampons, pads, and other menstrual products wearing breathable underwear removing wet clothes as soon as possible after working out or swimming not douching avoiding scented feminine products always wiping front to back after using the toilet keeping blood sugar under control avoiding hot tubs or hot baths Some medications can increase a person's chance of developing a vaginal yeast infection. These include antibiotics, birth control pills, and corticosteroids. People with weakened immune systems and those who are pregnant or breastfeeding are also at a higher risk of developing a yeast infection. Is sex safe with a yeast infection? When a person has a yeast infection, it is best to avoid sex. This is because partners can spread the infection to each other and pass the infection back and forth. Approximately 15% of males who have sex with someone with a vaginal yeast infection develop an itchy rash on their penis. Men living with diabetes and those with uncircumcised penises are at higher risk of developing a yeast infection. Condoms and dental dams may help prevent the spread of yeast infections between partners, but are not always effective for this type of infection. People should also let any of their sexual partners know if they have an infection so they can also seek treatment. Treatment If a person suspects they have a yeast infection, they should talk to a doctor, who can rule out other, potentially more severe infections. The typical course of treatment for a yeast infection is antifungal medication. Most people can buy over-the-counter (OTC) antifungal medication without a prescription from their local drug store. Treatments come in several forms, including pills, creams, ointments, and suppositories. The treatment can be a single dose or may be spread out over the course of a week. People can follow the directions on the packaging and ask a pharmacist if they have any questions. Some people experience recurrent yeast infections or those that do not go away with OTC treatments. If this is the case, a doctor may prescribe a stronger antifungal medication. Sometimes, a person will need to take antifungal medications for up to 6 months to help prevent future infections. Outlook A person can develop a yeast infection after sex if the sexual intercourse introduces a foreign body, such as bacteria, to the vagina. Yeast infections are not a major cause for concern. When a person experiences their first yeast infection, they may choose to get a diagnosis from their doctor. It is possible to treat most yeast infections with an OTC medication. People with active yeast infections should avoid sexual intercourse to help avoid spreading the infection. |
|
#222
|
||||
|
||||
|
Re: Sexual Health News
Is it normal to have a veiny penis?
By Jamie Eske https://www.medicalnewstoday.com/articles/326037.php In most cases, seeing veins beneath the skin of the penis is perfectly normal and does not require medical attention. Several factors influence vein visibility, including: genetics age frequency and intensity of physical activity cardiovascular health underlying medical conditions In this article, we discuss why the veins in the penis might appear prominent and what this means. We also review potential underlying medical conditions that contribute to penis vein visibility and when to see a doctor. Why does it happen? There are several veins and arteries that carry blood to and from the spongy erectile tissue in the penis. Veins may look larger than usual during and immediately following an erection. Although the appearance of prominent veins may cause alarm, they indicate healthy blood flow. Genetics and age can influence skin thickness, which may make veins appear more prominent or bigger than usual. Also, blood clots and other conditions that affect the cardiovascular system can trap blood in the veins, which may affect how these blood vessels look. Do prominent veins affect erection or ejaculation? Typically, prominent veins do not affect erectile function. Conditions that affect blood flow, such as blood clots and atherosclerosis, can have a minor impact on erectile function. Research suggests a close relationship between cardiovascular health and erectile function. In a 2015 study, for example, researchers conclude that erectile dysfunction could be an early sign of cardiovascular disease. Also, in an earlier study by the Heart Institute, the authors state that erectile dysfunction may precede heart attacks by 3–5 years. Possible causes Vein size and visibility may vary over a person's lifetime. They can also change as a result of sexual activity, or due to an underlying health condition. Some possible causes of prominent veins in the penis include: Erection During an erection, oxygenated blood from the heart flows through the cavernous artery, which supplies the three chambers of spongy tissue that make up the corpus cavernosum and the corpus spongiosum. The increase in blood flow causes the spongy tissue to expand, resulting in an erection. The tunica albuginea keeps blood in the corpus cavernosum. The blood will then drain through the veins near the surface of the penis and travel back to the heart and lungs. The spongy tissue will remain engorged with blood until the erection goes away. Varicocele A varicocele refers to enlargement of the veins that make up the pampiniform plexus in the scrotum, which is the loose skin that surrounds the testes. Varicoceles develop during puberty and affect about 10–15% of young males. The exact cause remains unknown, but the following factors may contribute to the formation of varicoceles: reduced blood flow swollen lymph nodes injury or trauma to the testes Varicoceles do not require treatment unless there is also: pain low sperm count a lump on or near the testes swelling of the scrotum Blood clots A blood clot, or thrombosis, is a medical condition that occurs when blood cells stick together to form solid masses in the blood vessels. Blood clots can interrupt or completely stop blood flow. Penile blood clots can develop in the dorsal vein in the penis, resulting in a rare condition called Mondor's disease. Mondor's disease can lead to significant pain and swelling in the affected veins. According to a 2018 case study, penile blood clots typically resolve on their own within 1–4 weeks. Lymphedema Lymphedema refers to swelling that occurs when lymph fluid incorrectly flows through the body. Swelling due to lymphedema can make the veins more visible than usual. Causes of lymphedema include: blockages in the lymphatic system cancer treatment infection injury removal of lymph nodes scar tissue buildup from surgery Peyronie's disease Peyronie's disease occurs when scar tissue, or plaque, forms in the top or bottom of the penis. The buildup of scar tissue can cause the penis to curve or bend, which can lead to severe pain during sexual intercourse. The scar tissue that develops may feel slightly firm to the touch. Scar tissue that calcifies can feel like a hard, solid mass beneath the skin. Causes of Peyronie's disease include: injury autoimmune disease vigorous sexual activity aging Lymphangiosclerosis The abnormal hardening of a lymph vessel in the penis characterizes lymphangiosclerosis. Lymphangiosclerosis can develop due to: injury causing tissue damage in the penis circumcision scarring from circumcision sexually transmitted infections vigorous sexual activity Unlike a prominent vein, lymphangiosclerosis will look similar to the rest of the skin. The hardened lymph vessel usually forms just below the head of the penis and measures about 3 millimeters thick. A doctor may perform blood tests and analyze a small tissue sample to diagnose lymphangiosclerosis. Lymphangiosclerosis typically goes away on its own within 4–6 weeks and rarely causes complications. People with lymphangiosclerosis should try to abstain from sexual activity, including masturbation until completely healed. When to see a doctor In most cases, a person will have no reason to worry if the veins in their penis appear more prominent than usual. However, people may want to consider speaking with a doctor if the appearance of veins in their penis causes them distress, or if they experience any of the following symptoms: pain during erection, ejaculation, or urination swelling of the penis or testicles hard, flesh colored cord on the penis lumps on the penis or scrotum pain in the lower abdomen or back If any of these symptoms occur alongside prominent veins in the penis, it may indicate an underlying medical condition. Summary The appearance of prominent veins in the penis may cause some concern. However, enlarged penile veins usually occur as the result of normal blood flow to and from the penis. In rare cases, an underlying medical condition can contribute to the appearance of penile veins. These conditions include: cardiovascular diseases, such as blood clots Peyronie's disease lymphangiosclerosis People may want to consider contacting their doctor if they have noticeable cord-like structures on their penis or testicles. People should seek immediate medical attention if they experience: painful erection or ejaculation swelling or lumps on the penis or scrotum pain in the lower back or abdomen unusual discharge from the penis |
|
#223
|
||||
|
||||
|
Re: Sexual Health News
What happens when you lose your virginity?
By Maria Cohut, Ph.D https://www.medicalnewstoday.com/articles/326122.php Losing your virginity is a unique experience. It can be hard to know just what to expect. What will it feel like, when should you do it, and how can you stay safe during your first time? The words "virginity" and "sex" mean different things to different people, regardless of whether they have sex with people of the same or different genders. Whatever definition people use, many feel anxious about having sex for the first time. This concern is totally normal, but rumors and myths that circulate among friends and on the internet can create unnecessary fears. Understanding what might happen during and after sex can help ease any worries. In this article, we look at what might happen both physically and emotionally when a person loses their virginity. We also tackle some common myths about virginity and sex and talk about how people can prepare for their first time having sex. What is virginity, and what is sex? Defining virginity is not straightforward sex and virginity can mean many different things to different individuals. When people say "virgin," they often mean a person who has not had penetrative, penis-in-vagina sex with another person. However, this is just one of many possible definitions. Not all people have penis-in-vagina intercourse. For them and for others, virginity loss may refer to their first time with oral sex, anal sex, or sex using fingers or toys. Some people feel that they have lost their virginity multiple times, by having different kinds of sex. Notions of virginity and sexual activity also differ among cultures. What happens to the body during sex? People usually notice physical changes during sexual activity. Some of these are the same for males and females, while other changes differ. Sex feels good because of both mental and physical factors. The brain releases hormones that support sexual pleasure, and there are thousands of nerve endings in the genitals that can feel good when stimulated. Learn more about why sex is pleasurable here. Before and during sex, the body releases hormones. These increase the amount of fluid in the vagina or stimulate the penis to become erect. A person may also feel their heart rate quicken and their body become more sensitive during sex. Does it hurt when you lose your virginity? Sexual contact may feel strange at first because it is an unfamiliar sensation. That said, sex including the first time should not be painful. To avoid discomfort, be sure to openly communicate with your partner before and during sex, telling them what does and does not work for you. If sex is painful, tell your partner and stop or try something different. To maximize pleasure and minimize the chance of discomfort, spend a lot of time on foreplay. This can mean kissing, caressing, teasing, or exploring. Foreplay will enhance arousal and prime you and your partner for an even more enjoyable experience. But even though foreplay and a state of arousal can help the vagina and penis self-lubricate, people may still need to add lubricant to prevent uncomfortable friction. Adding lube is a must during anal sex, as the rectum does not produce its own lubrication. Psychologist and sex educator Emily Nagoski, Ph.D., says that lubricant whether water-based or silicone-based should be a bedside staple for anyone who is sexually active. In her book, Come As You Are, Nagoski explains that lubricant helps reduce friction and increase pleasure. It also decreases the risk of any tearing and pain. Lube increases [the] efficacy [of protective barriers, such as condoms and dams] and makes them more pleasurable. Lube is your friend. Lube will make your sex life better. Emily Nagoski, Ph.D. A wide variety of lubricants provide different textures, sensations, and flavors. A person can find these at drugstores or choose between types online. What is the hymen, and how does sex affect it? One of the biggest myths about first-time vaginal sex is that a female's hymen a thin, elastic membrane that lines the opening of the vagina will break, causing bleeding and pain. People sometimes call this "popping the cherry." The hymen comes in many shapes and types, and some people are born without a hymen. During sex, the hymen can tear and cause minor bleeding. This is more likely to happen if the hymen is less elastic, such as during adolescence, or if it has a smaller opening. This bleeding is usually minimal. However, the hymen may not tear during sex. It is flexible and does not usually cover the entire vaginal opening. If it did, menstrual blood and other types of vaginal discharge would have no way of leaving the body. In many cases, a person's hymen has torn before they have sex. Some strenuous activities, such as sports, can cause minor tears in the hymen. Some people believe that a broken hymen is an irreversible sign of virginity loss. However, it is impossible to tell whether a person has had sex just by examining their hymen. This is because the hymen is naturally open in most cases and because its shape and size vary from person to person. The authors of a paper published in the journal Reproductive Health in 2019 say that healthcare professionals should never rely on physical examinations of the hymen to assess whether a person has become sexually active. Can losing your virginity damage your penis? Some people are worried that the frenulum which is the short band of tissue that connects the foreskin to the head of an uncircumcised penis can tear during first-time penetration. This is sometimes called "snapping the banjo string." This part of the penis is fragile. A person may tear it after having had sex many times or never the frenulum can tear during nonsexual activities, such as riding a bike. A torn frenulum can be painful and cause a small amount of bleeding, but this injury will heal on its own, just like any other minor cut or tear. If this happens, just carefully wash the area and gently pat it dry with a clean towel. Avoid activities that could cause the wound to open again until it has healed. When should you lose your virginity? People can feel a lot of pressure to have sex if they believe that there is a "right age," or if they feel like everyone else is doing it. However, many people take their time in deciding when or even if they want to become sexually active. The most recent data, collected in 2017, from the Centers for Disease Control and Prevention (CDC) show that 47.8% of high school students in the United States had never had any kind of sexual contact. So if you are worried about not having had sex don't be! There is no real right or wrong time to become sexually active. The right time is when it feels right for you that is, when you feel an enthusiastic desire to explore that part of yourself. If you never feel an urge to start having sex, that's absolutely fine, too. And if you feel like starting your sex life, but then decide you want to abstain from one, several, or all types of sexual activity for a while or forever that is also normal. Can you get an STI the first time you have sex? Yes. Every time a person has sexual contact without using barrier contraception such as condoms there is a chance they can develop a sexually transmitted infection (STI). This includes their first time. However, if neither person has had sexual contact with anyone else before, neither person will have an STI. Some STIs produce no symptoms, so a person may not know if they have one. To be sure, anyone who has had unprotected sexual contact before including oral sex or anal sex should have a sexual health screening. When it comes to preventing STIs, the best options involve physical barriers, such as female or male condoms, or dental dams for oral sex. People can get condoms from their healthcare provider or drugstores, or they can choose between types online. Most brands are safe to use. Learn about the safest condoms and tips for their use here, and learn how to choose the right condom size here. According to the American Sexual Health Association, 1 in 2 sexually active people will get an STI by age 25, and around half of STIs affect people aged 1524. The most common STIs include: human papillomavirus, better known as HPV chlamydia gonorrhea genital herpes Learn about the most common STIs and how to identify them here. Can you get pregnant the first time you have sex? Yes, if you are having penis-in-vagina sex. There are rumors that women cannot get pregnant when they lose their virginity, but this is not true. If you do not use contraception, penis-in-vagina sex carries a risk of pregnancy, even the first time. Some options for avoiding pregnancy include using male or female condoms, taking contraceptive pills, receiving a regular contraceptive shot, and having a doctor insert an intrauterine device, or IUD. What is consent, and why is it important? Consent means that each person involved in sexual activity has agreed to take part in it. If one partner is unsure whether they would like to have sex, or if they change their mind during sex, they should feel able to express this and to stop without any repercussions. For an enjoyable first-time experience, partners should feel safe, both emotionally and physically. If you feel pressured into doing more than you want, it is not going to lead to safe, enjoyable sex. If you are being coerced into having sex, tell this to someone you trust. People based in the U.S. can contact the Rape, Abuse, and Incest National Network hotlines, and this type of service is available in many other countries. How will I feel afterward? People sometimes feel that losing their virginity will be a life-changing experience. Each person's experience is different some may feel happy, emotional, relieved, anxious, or they may have no particular emotional response. There is no right or wrong reaction to having sex for the first time. How you feel could depend on the expectations that you had beforehand or on your personality, for example. Some people feel that having sex changes their relationship. The change can take on many forms and this is normal, too. Some people feel overwhelmed during or after sex. Remember that one sexual experience is just that a single experience as part of a greater context, and it does not have to shape your identity or life course. Future sexual experiences will all be different, depending on your growing experience of your body and sexual needs. Takeaway Losing your virginity does not need to be a stressful event. Understanding what to expect and what might happen can help a person prepare, both physically and emotionally, for losing their virginity in any way that is right for them. People decide to become sexually active at different ages, and some people never feel the urge. If someone does decide to have sexual contact, no visible physical changes can make a person stand out as sexually active. Finally, when having sex for the first time or any time consent is crucial. Also, communicate about what feels pleasurable and use adequate protection to avoid unwanted pregnancy and STIs. |
|
#224
|
||||
|
||||
|
Re: Sexual Health News
How to identify and treat a herpes skin rash
By Amanda Barrell https://www.medicalnewstoday.com/articles/326173.php Herpes is a common infection that the herpes simplex virus causes. One of the main symptoms is a rash of blisters that doctors sometimes refer to as a herpes rash. A herpes rash usually develops on the genitals or around the mouth but can occur nearly anywhere on the body. There are two types of herpes simplex virus (HSV) that cause a skin rash in different areas: HSV-1, or type 1, which typically causes orolabial herpes. It spreads in the saliva and tends to affect the area around the mouth and nose. HSV-2, or type 2, which typically causes genital herpes and usually spreads through sexual contact. The rash appears around the genitals. Sometimes it is also responsible for orolabial herpes. This article will explain the symptoms of a herpes skin rash and explore its causes and treatments. It will also examine some other possible causes of skin complaints that may look like herpes. What does a herpes skin rash look like? Herpes causes small sores to appear on the skin. These usually develop around the mouth and nose, but they can appear nearly anywhere on the body, including the fingers. Where the rash appears depends on where a person has acquired the infection. The first sign of a herpes outbreak tends to be a tingling, burning, or itching sensation in the area that it is affecting. This initial sign might occur a day or so before the sores appear. The sores can be tender, painful, and tingly. They look like clusters of small, fluid filled blisters that become pustules. For a few days to a week, they will break open, ooze fluid, and form a crust before healing over. The rash typically lasts from 710 days. The first time a rash appears, it may last for different lengths of time, depending on the type of herpes: oral herpes symptoms clear up in 23 weeks genital herpes symptoms clear up in 26 weeks When someone experiences a herpes outbreak for the first time, they may also suffer some or all of the following symptoms: fever swollen and red gums swollen lymph glands Once the virus is in the body, it invades the nerves that supply the area of the skin where it infected and stays there for life. There is no cure for the virus, which tends to reactivate and cause the symptoms of herpes from time to time. The first outbreak is usually the worst. While the symptoms of the virus do tend to come back every so often forever, they are not typically as severe. Learn more about what herpes looks like, with pictures, here Is it herpes or something else? Herpes rashes tend to look like clusters of small, fluid-filled blisters on a small area of the body. Other skin conditions that may resemble herpes include: Contact dermatitis An allergic reaction to an irritant can cause allergic contact dermatitis. Common irritants include antibiotic creams, cosmetics, shampoo, and perfumes. In babies, contact dermatitis may develop in the diaper area. Contact dermatitis can cause redness, swelling, and even blistering in the area it affects. Shingles Shingles causes a rash of blisters to appear on the skin. The same virus that leads to chickenpox, the varicella-zoster virus, causes shingles. The first sign of shingles tends to be a severe burning or tingling pain on one side of the body. A rash of fluid filled blisters follows a few days to a week later. The blisters tend to appear in one area of the body, most commonly one side of the trunk near the waistline. They may be tender to the touch or painful. The condition usually clears up within 35 weeks or sometimes less. Scabies An infestation of a microscopic parasite known as the human itch mite, or Sarcoptes scabiei causes scabies. The mite burrows into the skin to lay its eggs and deposits its waste products, or feces. Its presence causes an extremely itchy rash that looks like little pimples, creating red, scaly areas on the skin. Doctors use a class of medicines they call scabicides to treat the infestation. These are only available by prescription. Causes of herpes skin rash There are two types of HPV virus that causes herpes. While closely related, people contract them in different ways, although they both spread through body fluids and close human contact. The person who is the carrier of the virus does not need to be experiencing symptoms to be contagious. HSV-1 or oral herpes Most carriers of HSV-1 contracted it when they were infants or children. People can be spread through: skin-to-skin contact kissing sharing items such as lip balm, tableware, or toothbrushes HSV-2 or genital herpes Sexual contact tends to be how HSV-2 spreads. HSV-1 can also cause genital herpes, and it can spread in saliva during oral sex. The HSV-2 virus can also pass on to a baby during childbirth. Both forms of the virus enter the nerve cells of the body where they remain for life. The virus tends to lay dormant, or asleep, in the cells until something wakes it up and causes an outbreak of symptoms. Factors that can lead to an outbreak include: emotional stress illness fever exposure to the sun menstruation in females surgery Treatment There is no cure for herpes, but the sores will usually clear up on their own within a few weeks. Treatments that will shorten the duration of the outbreak and ease the symptoms are available. If a person gets frequent outbreaks, their doctor may recommend taking a pill every day for prevention reasons. This is known as "prophylaxis." Antiviral creams or ointments can relieve the burning, itching, or tingling. Antiviral pills can speed up the healing process. Both types of medicine tend to contain the same active ingredients. They include: acyclovir famciclovir valacyclovir People can get herpes medication from a doctor or pharmacist. Over-the-counter options are also available online. When to see a doctor For otherwise healthy people, a herpes skin rash is not usually anything to worry about unduly. The sores can be painful and uncomfortable but typically go away by themselves. Medicines to treat them are available from drug stores. The virus can cause complications in some people. Anyone with a long term health condition or weakened immune system who thinks they may have herpes should speak to a doctor. People living with cancer, HIV, or AIDS, or who have recently had an organ transplant should seek urgent medical help if they think they may have herpes. Anyone who suspects something other than herpes, such as dermatitis, shingles, or scabies, is causing their skin rash can talk to their doctor about a diagnosis. Summary Herpes is a common virus that can cause a rash of blistering sores on the skin. These tend to develop either around the mouth or genitals but can appear almost anywhere on the body. There is no cure for the virus, and carriers tend to suffer outbreaks at various times throughout their life. The clusters of fluid filled blisters may be unsightly and can be painful, but they are usually harmless. Antiviral treatments that can ease the symptoms and shorten the duration of an outbreak are available in drug stores. |
|
#225
|
||||
|
||||
|
Re: Sexual Health News
Men can protect themselves against penile, anal cancers with HPV vaccination
https://www.channelnewsasia.com/news...h-hpv-12065080 By Jalelah Abu Baker SINGAPORE: The incidence of penile and anal cancers in men in Singapore is low, but there is protection against these diseases in the form of vaccination against the human papillomavirus (HPV). READ: Commentary: HPV, the silent virus behind cervical cancer Deputy head and senior consultant in the Division of Medical Oncology at the National Cancer Centre Singapore Associate Professor Ravindran Kanesvaran told CNA that there have been 19 cases of penile cancer at the centre over the past five years, and 63 cases of anal cancer in men over the same period. READ: UK offers HPV vaccines to boys, aims to stop 100,000 cancer cases Certain strains of HPV can lead to these cancers in men, although the vaccination is typically encouraged for women as protection against cervical cancer. While HPV-related cancers are less common in men compared to cervical cancer in women, men will also benefit from HPV vaccination as it will prevent them from getting cancers like anal cancer, penile cancer and certain head and throat cancers, Dr Ravindran said. It will also reduce the risk of transmitting HPV to their female partners, he added. However, HPV vaccination for men has not been part of the national vaccination programme in many countries even though it has been included for women, he said. This is the situation in Singapore, where the Ministry of Health (MOH) has introduced fully subsidised school-based HPV vaccination programme for female secondary school students. BENEFITS OF VACCINATION SEEN IN BOTH BOYS AND GIRLS Dr Ida Ismail-Pratt, consultant in the Division of Gynaecologic Oncology at National University Hospital and National University Cancer Institute, Singapore said that in some countries like Australia, gender-neutral school HPV vaccination has been provided due to the benefit seen in both boys and girls. She added that in Singapore, two types of HPV vaccinations are licensed to be given to boys and men aged nine to 26 years for future protection from anal cancer, premalignant anal lesions and genital warts, although it is not covered by Medisave for men - unlike those for women. She said that males should go for HPV vaccination because there is currently no effective screening for HPV-related cancers other than cervical cancers, and the only way to protect males from anal cancer, penile cancer and oropharyngeal cancer- a type of head and neck cancer - is with HPV vaccination. Dr Tan Kok Kuan, chief medical officer at the Doctor Tan And Partners Clinics Group said that among eight clinics in Singapore, they vaccinate between 50 and 80 men a month against HPV. While he feels the awareness on HPV vaccination for men is certainly improving, he said there is space to educate men on the benefits of the vaccination, given that all disease awareness campaigns only mention HPV vaccination in the context of protecting women against cervical cancer. MISCONCEPTIONS SURROUNDING HPV VACCINATION FOR MEN Many men believe that HPV only causes cervical cancer and so it is exclusively for women, said Dr Tan. In fact, HPV is a virus that is just as infectious to men as to women, he said. Dr Ida echoed his point. It is as common as the flu virus. It is transmitted by skin to skin contact including sexual intercourse, she said. She said that while a majority of HPV infections are transient and can be rid of by the immune system, certain types can persist and increase the risk of HPV-related diseases. Another misconceptions is that it is only men who have sex with men that are at increased risk of HPV related cancers and pre-cancers, she said. The incidence of anal cancer and pre-cancer are not exclusively increased in men who have sex in men only, she said, adding that the the highest risk of anal cancer and precancer is seen in both men and women who are HIV-positive, practising anal receptive intercourse, and previous history of genital cancers or pre-cancers. MALES SHOULD CONSULT DOCTOR ON NEED FOR VACCINATION: MOH The Ministry of Health (MOH) said that in consultation with the Expert Committee on Immunisation (ECI), it takes into account criteria such as the disease burden in Singapore, the need for herd immunity as protection against outbreaks of potentially serious infectious diseases, and the clinical and cost-effectiveness of the vaccine, when including vaccines in the national schedules and school-based vaccination programmes. Cervical cancer is the tenth most common cancer, and eighth most common cause of cancer death among females in Singapore, a spokesperson said. As cervical cancer is mainly caused by the HPV, vaccination is recommended for females as it can protect against infection mainly from two of the HPV types that account for 70 per cent of cervical cancer cases. While HPV vaccination confers protection for prevention of genital warts, as well as some other cancers in males like anal, penile and oropharyngeal cancer, these cancers have low incidence rates in Singapore, she added. Males who have specific concerns on HPV infection or the risk of acquiring HPV should consult their doctor on the need for vaccination, MOH said. One male who has gone for the vaccination is 15-year-old Euan Lim. He is aware of the benefits that apply to men. The male receiving the vaccination will not just benefit himself. Therefore, it is an important vaccination for males to receive too, he said. Source: CNA/ja |
| Advert Space Available |
 |
| Bookmarks |
| Thread Tools | |
|
|
 t Similar Threads
t Similar Threads
|
||||
| Thread | Thread Starter | Forum | Replies | Last Post |
| Non sexual health question | sicknasty | Sexual Health Issues | 7 | 10-01-2015 05:45 AM |
| Sexual Health Issues | Whybother | Sexual Health Issues | 2 | 24-04-2013 07:02 AM |
| DSC Sexual Health Screening | Huluman | Sexual Health Issues | 3 | 23-11-2008 08:57 PM |
| Sexual Health & Well Being | MrDevil | Sexual Health Issues | 10 | 29-03-2004 09:36 AM |
| sexual health mentor | boyrusty2000 | Sexual Health Issues | 31 | 06-08-2003 11:10 PM |