
 |
|
|||||||
| Sexual Health Issues If you need medical advice regarding your sexual health, ask Dr Tan. We are honored to have an In House Doctor who is here to help. |
 |
|
|
Thread Tools |
|
#256
|
||||
|
||||
|
Re: Sexual Health News
Causes of heavy vaginal discharge
https://www.medicalnewstoday.com/articles/327379 Written by Jamie Eske on December 23, Regular vaginal discharge is a sign of a healthy female reproductive system. Normal vaginal discharge contains a mixture of cervical mucus, vaginal fluid, dead cells, and bacteria. Females may experience heavy vaginal discharge from arousal or during ovulation. However, excessive vaginal discharge that smells bad or looks unusual can indicate an underlying condition. This articles discusses why someone may have heavy vaginal discharge and what they can do about it. 1. Arousal Arousal, ovulation, and hormonal imbalances can each cause heavy discharge. Sexual arousal triggers several physical responses in the body. Arousal increases blood flow in the genitals. As a result, the blood vessels enlarge, which pushes fluid to the surface of the vaginal walls. Arousal fluid is clear and watery with a slippery texture. This fluid helps lubricate the vagina during sex. Other signs of female arousal include: increased heart rate and breathing flushing of the face, neck, and chest swelling of the breasts erect nipples 2. Ovulation Cervical fluid is a gel-like liquid that contains proteins, carbohydrates, and amino acids. The texture and amount of cervical fluid both change throughout a female’s menstrual cycle. For example, after menstruation, cervical fluid has a thick, mucus-like texture. It can be cloudy, white, or yellow. Estrogen levels increase closer to ovulation. This causes the cervical fluid to become clear and slippery, similar to that of raw egg whites. Cervical fluid discharge increases during the days leading up to ovulation and decreases after ovulation. Females may have no discharge for a few days after their period. 3. Hormonal imbalances Hormonal imbalances related to stress, diet, or underlying medical conditions can cause heavier vaginal discharge. Polycystic ovary syndrome (PCOS), for example, refers to a set of symptoms that occur as a result of hormonal imbalances. According to the Centers for Disease Control and Prevention (CDC), PCOS affects up to 5 million females in the United States. Those with PCOS have higher levels of male hormones called androgens. Increased androgen levels can: change the amount or texture of cervical fluid cause irregular periods prevent ovulation Not everyone with PCOS will have increased vaginal discharge. Paying attention to other PCOS symptoms may help someone identify and seek treatment for the condition faster. Some other symptoms of PCOS to look out for include: fewer than eight periods in 1 year, or periods that occur every roughly 21 days excess facial and body hair thinning hair or hair loss acne on the face and body weight gain darkening of the skin on the neck, groin, or breasts skin tags on the armpits or neck Hormonal birth control, such as birth control pills and intrauterine devices, can also cause increased vaginal discharge, especially during the first few months of use. Excess vaginal discharge and other symptoms, such as spotting and cramping, usually resolve once the body adjusts to the hormonal birth control. 4. Vaginitis Vaginitis refers to inflammation of the vagina, which can occur from an infection or irritation due to factors such as douches, lubricants, and ill-fitting clothing. Vaginitis can cause thick vaginal discharge that may be white, gray, yellow, or green. Other symptoms of vaginitis include: foul vaginal odor an itching or burning sensation in the genital area redness or inflammation of the vagina pain or discomfort when urinating pain during sexual intercourse 5. Bacterial vaginosis Bacterial vaginosis is a condition that results from an overgrowth of bacteria in the vagina. This vaginal infection is the most common among females aged 15–44 years. The exact cause of bacterial vaginosis remains unclear. Females can develop bacterial vaginosis after sexual intercourse. However, this condition is not a sexually transmitted infection (STI). According to the Office on Women’s Health, those who have bacterial vaginosis may notice a milky or gray-colored vaginal discharge. Some also report a strong, fishy vaginal odor, especially after sexual intercourse. Bacterial vaginosis can also cause: discomfort when urinating painful burning or itching in the vagina irritation of the skin around the vagina 6. Yeast infection Vaginal yeast infections result from an overgrowth of the Candida fungus. Females of all ages can develop a vaginal yeast infection, and nearly 70% will have a yeast infection at some point in their lives. The most common symptom of a vaginal yeast infection is an intense itching in the vagina and vulva. Vaginal yeast infections can also cause an odorless vaginal discharge that looks similar to cottage cheese. Vaginal yeast infections are treatable at home using over-the-counter antifungal ointments. Symptoms should improve within a few days. However, severe infections can last longer and may require medical treatment. 7. Trichomoniasis Trichomoniasis is an STI caused by a parasite. Females can develop trichomoniasis after having sex with someone who has the parasite. Although most people who have trichomoniasis do not experience symptoms, some may have an itching or burning sensation in the genital area. Trichomoniasis infections can also cause excess vaginal discharge that has a foul or fishy odor and a white, yellow, or green color. It may also be thinner than usual. What is healthy discharge? Healthy vaginal discharge varies from person to person. It also changes throughout their menstrual cycle. In general, healthy vaginal discharge can appear thin and watery or thick and cloudy. Clear, white, or off-white vaginal discharge is also perfectly normal. Some females may have brown, red, or black vaginal discharge at the end of their menstrual periods if their vaginal discharge still contains blood from the uterus. Natural hormonal changes during ovulation can cause an increase in vaginal discharge, which should return to normal after ovulation. When to see a doctor It is not always necessary to see a doctor about excessive vaginal discharge. However, a female may want to consider seeing their doctor if their vaginal discharge has an abnormal appearance. Yellow, green, gray, or foul-smelling vaginal discharge could indicate an infection. Other reasons to see a doctor include: itching or burning near the genitals discomfort or pain when urinating discomfort or pain during sexual intercourse Possible treatment options Treating excess vaginal discharge depends on the underlying cause. People can reduce symptoms of vaginitis by avoiding the source of irritation. Doctors can treat bacterial vaginosis and yeast infections using antibiotics or antifungals. Doctors can also treat trichomoniasis using antibiotics. The CDC recommend that females wait 7–10 days after receiving treatment before having sex. Treatment for PCOS varies depending on the individual. A doctor may recommend a combination of lifestyle changes and medications to help people manage their symptoms and regulate their hormone levels. Maintaining a healthy body weight and eating a varied diet low in added sugars may also help improve some symptoms of PCOS. Birth control pills that contain estrogen or progestin can help balance out excess levels of androgens. Tips for managing heavy vaginal discharge Even healthy vaginal discharge can cause discomfort at times. Here are some tips for managing heavy vaginal discharge: Wear panty liners. However, be sure not to let them become too moist, as this can increase the risk of urinary tract infections and vaginitis. Choose breathable underwear made from natural fibers such as cotton. Avoid wearing tight pants. Avoid using hygiene products that contain added fragrances, coloring agents, or other harsh chemicals. Keep the genital area clean and dry. Wipe from the front to the back when using the bathroom. Outlook Excess vaginal discharge can occur as a result of arousal, ovulation, or infections. Normal vaginal discharge ranges in color from clear or milky to white. The consistency of vaginal discharge also varies from thin and watery to thick and sticky. Generally, healthy vaginal discharge should be relatively odorless. A female can speak with a healthcare professional if they notice any symptoms of an infection. Some symptoms to look out for include: yellow, green, or gray vaginal discharge foul-smelling vaginal discharge discharge that looks similar to cottage cheese itching or burning in or near the genitals Doctors can easily treat most vaginal infections using antimicrobial medications. Depending on the severity of the infection, people may see their symptoms improving within a few days to weeks. |
|
#257
|
||||
|
||||
|
Re: Sexual Health News
'JUST DEVASTATING' Mum shares shocking pics of six-month-old baby daughter who contracted herpes
https://www.thesun.co.uk/news/110833...-pictures/amp/ By Lucy Laing 2nd March 2020, 8:30 pm Updated: 3rd March 2020, 7:03 am DISTRESSING images show a baby girl with herpes — a virus which can be transmitted by a single kiss. Little Oarlah was rushed to hospital aged just six months amid fears she could go blind. She contracted the virus despite mum Hollie Cruickshanks imposing a kissing ban after her birth. Viral spots and sores spread from Oarlah’s body, across her head and face and even got into her left eye.    Hollie, 21, said: “When I saw those, I was filled with horror. I knew she could be blinded because of it. “The thought of her losing her sight was just devastating.” Oarlah was on a drip in hospital while Hollie and partner Bradley Airlie, 21, faced an anxious wait for news. Luckily, tests showed the tot’s eyesight was not damaged and the swelling reduced after 24 hours. Hollie, from Dundee, gave birth in November 2018. ‘FILLED WITH HORROR’ While pregnant, she saw a post on Facebook from a mum whose baby caught herpes from a kiss. Hollie said: “I was horrified. People thought I was paranoid when I said I didn’t want anyone kissing Oarlah but I’d seen what it could do. “I couldn’t help myself and I kissed her on the forehead when she was born, but then I banned all her visitors from kissing her. “I tried to protect her and she still got this horrible virus but the doctors told us that it could also be transferred on the hands too.” Hollie says Oarlah, now 15 months, has made a full recovery, but added: “I still don’t let anyone kiss her. “It was just bad luck she got this. We feel very lucky she came through it.” Unwise to kiss if sick By Carol Cooper, Sun Doctor HERPES viruses are very contagious and the first time a person catches it is usually the worst.Around 90 per cent of people are thought to carry herpes, but very few babies catch it.When my children were young, I was reluctant to let people kiss them.It’s certainly unwise to kiss or touch a baby if you have an active infection of anything. |
|
#258
|
|||
|
|||
|
Re: Sexual Health News
It's scary. My hair all stand up. Sad for the baby
|
|
#259
|
||||
|
||||
|
Re: Sexual Health News
HSA issues alert over 3 'sexual enhancement' products, including coffee sold at Bedok North eatery
https://www.channelnewsasia.com/news...-shop-12570036  SINGAPORE: The Health Sciences Authority (HSA) issued an alert on Tuesday (Mar 24) warning members of the public about three products containing "potent medicinal ingredients" used to treat erectile dysfunction. Two of the products - Kopi Jantan Ali Macca and Kopi Panggung AL-Ambiak Natural Herbs Coffee - were sold at a coffee shop along Bedok North Street 3. The latter was also sold on local e-commerce platforms, marketed as a "performance-enhancing coffee". Acting on feedback from a member of the public, HSA found that the two coffee products were sold at Shaik Abdul Kader Al-Jailani Makan Place coffee shop in Bedok North. Subsequents tests showed that Kopi Jantan Ali Macca contained a potent medicinal ingredient called sildenafil, while Kopi Panggung AL-Ambiak Natural Herbs Coffee contained a different ingredient called desmethyl carbodenafil. Such potent medicinal ingredients can seriously harm people's health, said HSA. The third product, Berry Jaga Chewable Candy, was found to contain up to 10 times the usual daily dose of tadalafil, which is normally prescribed for erectile dysfunction. 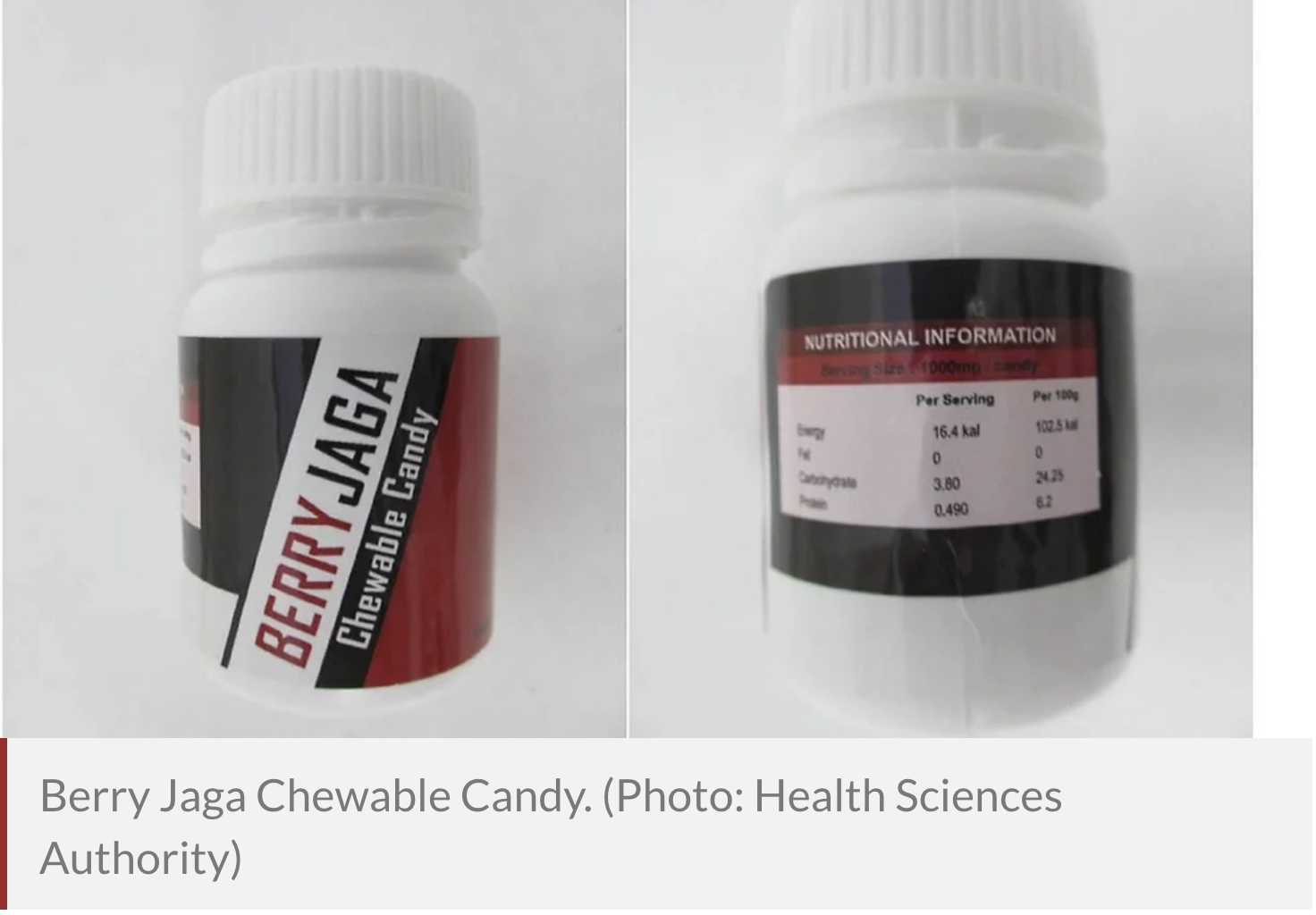 The candy was marketed for sexual enhancement on Berry Jaga Marketing's website and local e-commerce platforms. It was labelled as containing fruit juice powders, but its marketing included cautionary advice, recommending that consumers with medical conditions such as low blood pressure, heart issues or those who take medicines such as nitrates not consume the product. "This is usually a tell-tale sign that the product may contain potent medicinal ingredients," said HSA. Sildenafil and tadalafil are prescription medicines used to treat erectile dysfunction and should only be used under medical supervision, said the authority. If used inappropriately, they could cause a stroke, heart attack, low blood pressure and priapism (painful and exceedingly long erections). Desmethyl carbodenafil is chemically related to sildenafil and may cause similar adverse effects or "even more toxic ones", added HSA. The medicines should not be used by patients taking heart medication - especially nitrates - as this can cause potentially life-threatening low blood pressure. HSA said it has directed Shaik Abdul Kader Al-Jailani Makan Place and Berry Jaga Marketing to stop the sales of the respective products and is working with local e-commerce platform administrators to take down the affected listings. Consumers are advised to stop taking the three products immediately and should go see a doctor if they feel unwell, said the authority. "All sellers and suppliers must stop selling these products immediately," it added. "It is illegal to sell and supply such products which contain potent medicinal ingredients." If convicted, sellers and suppliers could be jailed for up to two years and/or fined up to S$10,000. |
|
#260
|
||||
|
||||
|
Re: Sexual Health News
Benefits and risks of circumcision
https://www.medicalnewstoday.com/articles/302234 Circumcision is an operation to remove a male’s foreskin. It is one of the oldest and most common surgical procedures. A male may undergo this procedure for religious, social, medical, or cultural reasons. The Centers for Disease Control and Prevention (CDC) encourage male circumcision on the basis that it appears to reduce the risk of HIV infection during vaginal sex. However, not all health authorities agree, and the recommendations remain somewhat controversial. Circumcision is fairly common in the United States. In fact, according to the CDC, 58.3% of U.S. newborns underwent circumcision in 2010. It is less common in other Western countries, however. In the United Kingdom, for example, only around 8.5% of males are circumcised. This article will discuss what to expect during the procedure itself, as well as some possible benefits and risks. What is circumcision? Circumcision involves the removal of the foreskin of the penis. The foreskin is the shroud of skin that, when gently pulled back, uncovers the head of the penis. The surgery is relatively simple. A healthcare professional will free the foreskin from the head of the penis and, in newborns, clip it off in a procedure that only takes a few minutes. In adults, they will remove the foreskin with a scalpel, and it takes around 30 minutes. They will then either cauterize or stitch the wound with dissolvable sutures. History The first circumcisions may have taken place around 15,000 years ago. The procedure then slowly spread across a variety of cultures, especially in the Middle East. It may have become popular in the ancient world as a public health measure and a way of preventing balanitis. Balanitis leads to swelling and pain in the head of the penis. This condition might have been more common in ancient societies due to sand building up under the foreskin. Circumcision became popular in the Western world in the late 19th century, when people began performing the operation in an attempt to prevent masturbation. Many believed that masturbation was associated with conditions such as epilepsy, paralysis, tuberculosis, and insanity. However, there was little compelling evidence to support these claims. As the newly formed national healthcare systems started facing rising costs, they stopped recommending the procedure. In the U.S., however, it has remained a relatively common practice, and some major health authorities do still encourage it. Why circumcise newborns? A number of factors are associated with neonatal circumcision. The most common are: religion hygiene health considerations Some studies have suggested that circumcision reduces the risk of urinary tract infection, but more recent findings have contradicted this, with some suggesting that it might actually increase the risk. Evidence has indicated a lower risk of some sexually transmitted infections (STIs), including syphilis. Circumcised males also appear to be less likely to contract herpes or HIV. In very rare cases, balanitis or phimosis can develop in an uncircumcised male. With these conditions, the foreskin cannot retract. This requires surgical treatment. Cancer of the penis is extremely rare, but it appears to be slightly more common in males with a high body mass index (BMI), males with a history of smoking, males who are uncircumcised, and those with a combination of these factors. Adult circumcision Circumcision is less common in adults than in children. It takes longer and is likely to involve more tissue trauma. It may also cause more psychological trauma than it does in newborns. However, it may reduce the risk of certain conditions, including phimosis, paraphimosis, and balanitis. Phimosis is the inability to pull back the foreskin, leading to pain and urinary problems. It can occur if a male is born with a tight foreskin, or due to scarring, infection, or inflammation. Treatment options include topical corticosteroids or circumcision. Paraphimosis occurs when the foreskin becomes stuck behind the head of the penis and restricts blood flow to the end of the penis. It can result from a medical intervention, such as the use of a catheter. Paraphimosis is a medical emergency. Without treatment, gangrene can result. Treatment aims to reduce the swelling, but most doctors recommend circumcision after recovery, in order to prevent the condition reoccurring. Balanitis occurs when the head of the penis becomes inflamed or swollen. This may be due to an STI, thrush, skin irritation, or another skin condition. It is uncommon in circumcised males. Circumcision can prevent balanitis reoccurring. Circumcision and HIV According to the World Health Organization (WHO), there is “compelling evidence” to suggest that circumcision reduces the risk of contracting HIV during vaginal sex by 60%. However, they point out that circumcision will offer only partial protection, and they urge people to use barrier methods such as condoms as well. The higher chance of infection may be because the foreskin becomes more prone to splits and ruptures during intercourse, allowing pathogens to enter the bloodstream. Another possibility is that the space between the penis and the foreskin might provide an environment in which a virus can survive for a period of time, raising the risk of infection for the individual and their next partner. Some argue that the U.S. has a relatively high rate of HIV despite high circumcision rates. In addition, the results of studies in Africa and Asia associating circumcision with HIV prevention, mainly in heterosexual populations, may not translate to the U.S. Risks Circumcision is a relatively safe procedure, and severe complications are rare. However, the following risks are possible: The surgeon cuts the foreskin too short or leaves it too long. The wound does not heal properly. Blood loss and hemorrhage occur. Meatal stenosis occurs. This condition causes the urinary stream to be deflected upward, making it difficult to aim. Damage affects the urethra, which is the tube that carries urine through the penis. This can make urination difficult. In very rare cases, there may be accidental amputation of the head of the penis. Blood infection or poisoning, known as septicemia, may develop. The foreskin left behind might reattach to the penis and require further minor surgery. There may be a decrease in the sensation of the penis, especially during intercourse. Complications are more likely when: an older male undergoes the procedure the procedure takes place in unsterile conditions inexperienced or untrained providers carry out the procedure the procedure takes place in a traditional manner, as a rite of passage If a qualified medical professional carries out the procedure in a sterile environment, the risks are minimal. Psychological effects Psychologists have expressed concern about the psychological effects of male circumcision. The procedure may be psychologically traumatic, especially to infants, children, and teenagers. Infants often undergo surgery without anesthesia, and this can lead to recurring pain and brain changes linked to mood disorders. Some males have experienced depression, anger, and intimacy problems stemming from the fact that this procedure took place in infancy without their consent. Older children can experience a degree of trauma with any surgical intervention, and this is particularly the case if it involves the genitals. In adolescence, it can lead to symptoms of post-traumatic stress disorder. In males with phimosis, using less invasive methods — such as a corticosteroid cream — may help reduce the risk of anxiety and castration anxiety that circumcision could entail. Parents and caregivers, as well as older males, can use an online circumcision decision maker to help them decide whether or not to consider the operation. Recovery The area will be bruised and swollen for several weeks, and urination may be painful for a few days or weeks. Some discomfort normally occurs after circumcision, but the pain is not usually severe, as this is a fairly minor operation. Pain medication can help. Recommendations for the recovery period include: wearing underwear that holds the penis in place, rather than loose-fitting boxer shorts drinking plenty of fluids, to dilute the acidity of the urine and reduce pain during urination avoiding physical activity until the wound has healed not using an antiseptic cream or other cream not provided by a doctor, as this can interfere with the healing process and increase the risk of infection and scarring Applying a little petroleum jelly to the end of the penis may reduce the stinging sensation during urination. Erections can also be painful during the recovery phase. To minimize the chance of nocturnal erections: Empty the bladder before going to bed, and use the bathroom as necessary during the night. Lie on one side, rather than on the back. Try drawing the knees up into a fetal position. Summary Circumcision is usually a simple operation, with a relatively low risk of complications. However, it is not always a simple decision to make. It is worth remembering that the American Academy of Pediatrics, while recommending circumcision for certain health reasons, note that this procedure should be “for families who choose it,” not a routine operation for all male infants. |
|
#261
|
||||
|
||||
|
Re: Sexual Health News
Top 10 things you didn't know about your penis
https://www.medicalnewstoday.com/articles/320748 Although many of us men are relatively familiar with our penis and its antics, there’s more to our appendage than meets the eye. In this feature, we discuss 10 interesting things that you probably didn’t know about your genitals. whatever you happen to call it — todger, wang, willy, or dangler — the penis is an odd-looking bit of kit. But beyond the japes and sniggers, it is, of course, vital to the survival of our species. When you consider the penis as an evolutionary adaptation, it has done remarkably well. We can all say without too much doubt that our father’s penis worked, as did our grandfather’s, and his father’s, and so on, right back through successive generations until we reach far beyond the birth of humanity. The penis is ancient. Just in case you were wondering, the oldest known penis dates back 425 million years, and its fossilized remains belong to an arthropod dubbed Colymbosathon ecplecticos, which means “amazing swimmer with a large penis” in Greek. It’s worth reflecting on its role in our species’ survival next time you are surprised by how easily your penis is “activated.” As far as reproduction is concerned, a false arousal is better than a missed opportunity. As the author Mokokoma Mokhonoana once wrote, “Even the world’s greatest actor cannot fake an erection.” This leads us on to the first penis fact of the day. 1. Your first erection Penises are born ready. It is common for babies to exit the womb with an erection. Even before the moment of birth, ultrasound scans sometimes show a fetus with a fully formed erection. According to a study from 1991, fetal erections occur most commonly during random eye movement (REM) sleep. And, they can happen a number of times each hour. No one is quite sure why, but it might just be our body’s way of testing things out and keeping them running correctly. 2. Your penis is twice as long as you think A lot of men might take solace in this fact: our penises are longer than they look. In fact, around half of its entire length is housed inside of our bodies.  3. The shoe size myth Let’s lay this one to rest, shall we? According to a study published in the journal BJU International, there is no correlation between shoe size and penis length. Although an older study — which was published in 1993 — did find that penile length was related to both height and foot length, it was a weak relationship, and the authors concluded, “Height and foot size would not serve as practical estimators of penis length.” Also, the International Journal of Impotence Research published an Iranian study looking at other correlations. They concluded that “penile dimensions are significantly correlated with age, height, and index finger length,” but not foot size. 4. ‘Morning wood’ Most men have 3–5 erections every single night — mostly during REM sleep, as with the in utero boys. Also called nocturnal penile tumescence, it’s still not clear why it happens. However, one theory is that it might help to prevent bed-wetting; an erection inhibits urination. A full bladder is known to stimulate nerves in a similar region to those involved in erections. But because females experience something similar — nocturnal clitoral tumescence — bed-wetting prevention is probably not the entire answer. Another potential explanation is that REM sleep is linked with switching off cells that produce noradrenaline in the locus coeruleus, which is in the brainstem. These cells inhibit the tone of the penis. So, by reducing the inhibition, the penis becomes erect. Whatever the reason behind nocturnal erections, they can be useful as a diagnostic tool. If a man has difficulty achieving an erection when awake but becomes erect when he sleeps, it is an indication that there is a psychological issue, rather than a physical one. However, if he does not get erections during sleep, the issue may be physical. 5. One final erection So, we’ve established that we can get erections in the womb and during sleep, but this is perhaps even more surprising: the death erection. Also called angel lust or terminal erection, it happens in the moments after death. Most commonly, it occurs in men who have died from hanging; scientists believe that it may be due to pressure from the noose on the cerebellum. However, it has also been reported following death by a gunshot wound to the head, damage to major blood vessels, and poisoning. 6. You can break your penis As I’m sure you are aware, there is no bone in your penis, which is fairly unusual for mammals. However, it is still possible to break your penis. It most commonly occurs during vigorous sex, although it has been documented to happen to men who fell out of bed with an erection. Penile fracture, as it is known, is actually the rupture of the fibrous covering of the corpora cavernosa, which is the tissue that becomes erect when engorged with blood. The moment of fracture is accompanied by a popping or cracking sound, intense pain, swelling, and — unsurprisingly — flaccidity. Thankfully, it doesn’t happen very often and, if it is treated swiftly, full function can be restored. As a note of caution, if this happens to you, don’t let embarrassment get the better of you. Go and get it sorted as soon as possible. In a study that investigated 42 cases of penile fracture, the most “dangerous” position was defined as “woman on top.” 7 . No-brainer Most men have very little control over exactly when they ejaculate. This is partly because it does not involve the brain. The signal to ejaculate comes from the spinal ejaculation generator. This region in the spinal cord coordinates the necessary functions. Of course, the higher brain does have some input into these matters — thinking about something else is a well-known way to delay the event, for instance — but the nuts and bolts of the whole operation are dealt with in your spine. 8. The angle of the dangle A man’s erection can point in virtually any direction. Straight ahead, left or right, up or down, there’s no right or wrong. The following data come from a study that measured the erections of 1,565 men. In the figures below, if the penis pointed directly up, it was measured as 0 degrees, and if it was forward-pointing (horizontal), it would be 90 degrees: 0–30 degrees — 4.9 percent of men 30–60 degrees — 29.6 percent of men 60–85 degrees — 30.9 percent of men 85–95 degrees — 9.9 percent of men 95–120 degrees — 19.8 percent of men 120–180 degrees — 4.9 percent of men So, if you’ve ever been concerned that your chap is a bit skew-whiff, don’t worry — you’re normal. While we’re on the topic of “normality,” very few penises are straight; they can curve in any direction. A curve of up to 30 degrees is still considered normal. 9. Grower or show-er A study on 274 men demonstrated that there is no correlation between the length of a flaccid penis and its erect size. Some start small and end up large (a grower), while some are large when flaccid and only grow a little when erect (a show-er). Some are even small whatever state they are in, and some are large when flaccid and get much larger. It’s a mixed bag. This doesn’t hold much relevance outside of the locker room, but I guess it’s good to know anyway. 10. Cornflakes prevent masturbation They don’t, really. However, Dr. John Harvey Kellogg — the breakfast cereal mastermind — hoped that they would. He invented these and other products because he thought that plain foods would lead Americans away from the “sin” of masturbation. Thankfully, nowadays, food manufacturers spend less time trying to convince the youth to give up masturbation. And, just in case there was any doubt, it doesn’t make you go blind, either. If this little list has tickled your fancy, your next move might be to plan a trip to Iceland and visit the Icelandic Phallological Museum. It is dedicated to all things penile; it was started up by Sigurður Hjartarson after being given a bull’s penis as a boy. According to Hjartarson, “Collecting penises is like collecting anything. You can never stop, you can never catch up, you can always get a new one, a better one.” Or, if you want to go one step further, you can visit the Guolizhuang Restaurant in Beijing, China, which specializes in penis and testicle dishes. It’s up to you. |
|
#262
|
||||
|
||||
|
Re: Sexual Health News
What is the refractory period, and can you reduce it?
https://www.medicalnewstoday.com/art...ractory-period The refractory period is the span of time after having an orgasm during which a person is not sexually responsive. The refractory period can have both mental and physiological effects. During the refractory period, a person might lose interest in sex, or they might not be able to have sex. It may not be possible for a person to get an erection, ejaculate, or orgasm. Scientists have thoroughly documented the refractory period in males. In females, the refractory period is more controversial. What happens in the refractory period? Doctors define the resolution stage of sex as when a person feels satisfied, usually following orgasm or, in the case of males, ejaculation. The refractory period occurs after the resolution stage. During the refractory period, a male cannot get an erection. This type of response is a physiological refractory period, meaning a person is physically unable to have sex again. Unlike males, many females can have multiple orgasms, suggesting they do not usually experience a physiological refractory period. Additionally, a female’s genitals may remain lubricated after sexual activity even if she no longer feels aroused, making sexual intercourse easier. However, both males and females can experience a psychological refractory period. This psychological type happens when a person does not want to have sex again. They may feel satisfied and prefer to avoid immediate sexual contact. Some people also feel tired during this period. Brain imaging studies suggest that the cycle of a sexual response follows a similar pattern to other pleasurable activities. It begins with intensifying desire, culminates in satisfying that desire, and concludes with decreased desire. Refractory period for males During the refractory period, a male is unable to get an erection or ejaculate again. This physiological response usually accompanies a psychological refractory period, during which the person feels uninterested in sex. The length of the refractory period varies greatly from person to person, from a few minutes to 24 hours, or longer. Researchers do not fully understand what causes the refractory period or why it varies so much in duration from person to person. Additionally, not all males have a refractory period. An older 2002 report on a 25-year-old male who did not experience any refractory period found that he did not secrete the hormone prolactin after ejaculating, as most males do. This finding suggests that prolactin may play a role in determining whether a male can have multiple orgasms. However, as this was a small study, and females also produce more prolactin after orgasm, researchers need to continue investigating. Similarly, some males find that they can orgasm without ejaculating, allowing them to have multiple “dry” orgasms and no refractory period. Refractory period for females While some females lose interest in sexual activity after an orgasm, they are usually physically able to engage in sexual activity again. However, some women do report a physiological refractory period. One study from 2009 showed that after orgasm, a female’s clitoris can become too sensitive to continue sexual activity. Out of 174 females, 96% reported this symptom, and many did not want to have sex again as a result. Most of the research into refractory periods to date has focused on males, so scientists know much less about the female response. Scientists will need to conduct more research to understand a greater variety of perspectives. Changes with age Sexual function tends to decline with age. People may need longer to get both physically and psychologically aroused as they grow older. They may also need longer to recover from sex, which may mean a more extended refractory period. The refractory period a person has when they are young will also determine how it changes as they age. Someone with a long refractory period as a teenager may find it continues to get longer over time. Factors affecting the refractory period Many factors can influence the length of the refractory period, including: a person’s overall health relationship quality quality of sex frequency of sex Dopamine plays a key role during sex. A review of the research suggests that dopamine levels may influence whether a male can get an erection. However, the review also notes that too much dopamine could cause sexual health problems as well. Some of the same activities that improve overall health, such as exercise, may help regulate dopamine levels. Other pleasurable activities may also boost dopamine, such as doing something new, enjoyable conversation, or mastering a new challenge. Scientists do not completely understand the connection between dopamine levels and the refractory period. Reducing the refractory period The internet offers plenty of advice about how to shorten the refractory period. While message board strategies may work for some people, there is usually little research to prove they work. The same strategies that improve overall health may boost sexual health. Cardiovascular health, in particular, correlates with sexual health. A person who wants to improve their overall wellbeing and sexual function can try: doing cardiovascular exercise, such as walking, running, or aerobics maintaining a healthy body weight eating a nutrient-dense diet treating or managing underlying health conditions, such as diabetes Some people try pelvic floor exercises to try and shorten the refractory period. People refer to these exercises as Kegels or pelvic floor muscle training (PFMT). So far, no research exists to prove that PFMT will shorten the refractory period. However, it may improve sexual function more generally in males and females. To try PFMT, a person should tense the muscles they use to urinate, hold for a few seconds, release, and repeat. Some research has found that erectile dysfunction medication might shorten the refractory period for males. A small, older 2003 placebo-controlled trial found that 40% of males participants reported a significant reduction in the refractory period when they used sildenafil (Viagra). Just 13.3% of placebo users experienced a similar reduction. However, another 2005 placebo-controlled, double-blind study found that Viagra did not shorten the refractory period. Summary The refractory period varies from person to person. While the refractory period tends to increase with age, other factors may influence the time a person cannot have sex again, such as their cardiovascular health. People can try easy techniques, such as PFMT if they wish to shorten the refractory period, but it is unclear if this can help. A doctor or therapist specializing in sexual health may suggest other strategies to improve overall sexual function. |
|
#263
|
||||
|
||||
|
Re: Sexual Health News
HSA raises alert on 2 products, including coffee product with high levels of erectile dysfunction medicine
https://www.channelnewsasia.com/news...power-12773714 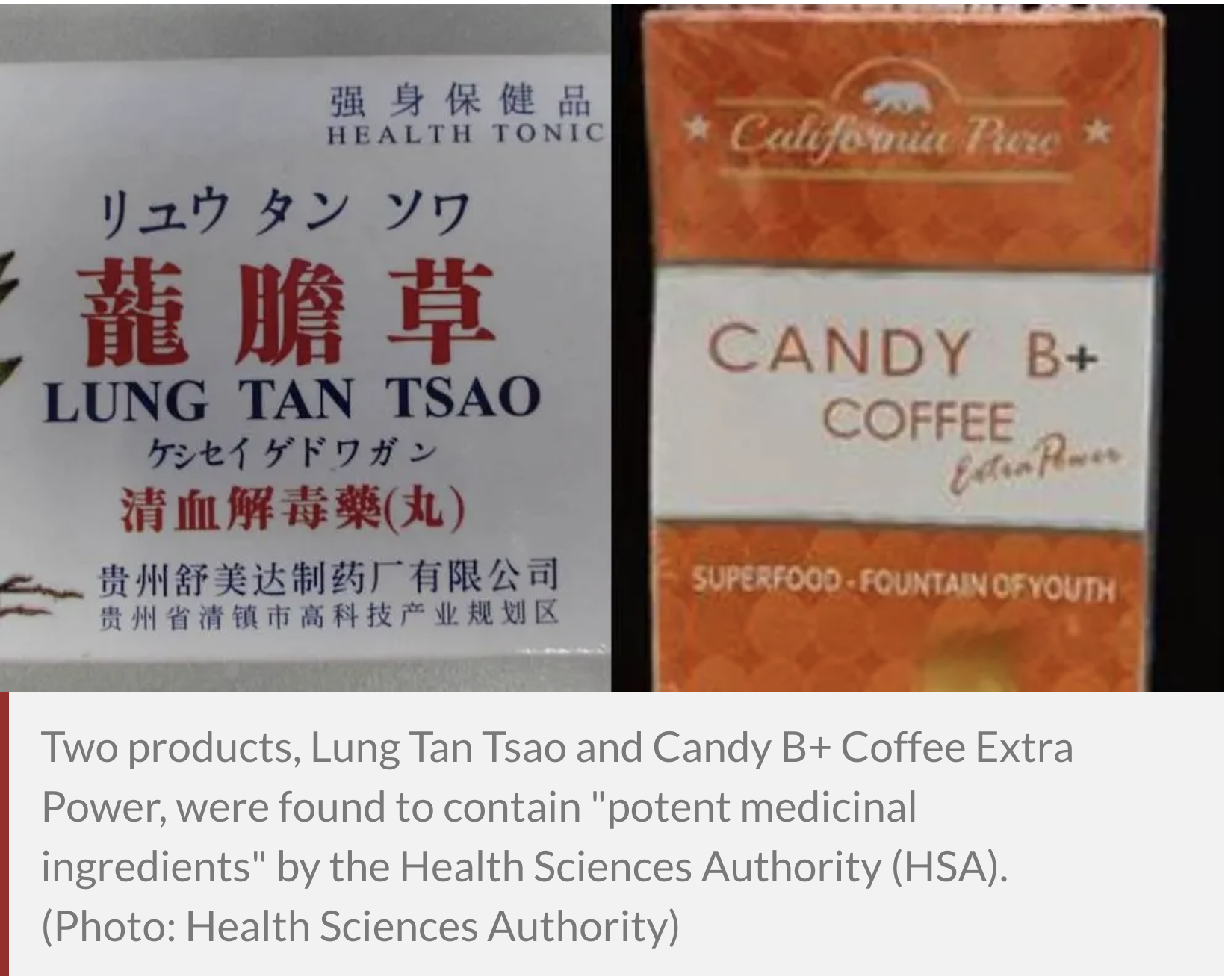 SINGAPORE: Members of the public have been warned against purchasing or consuming two products found to have "potent medicinal ingredients", the Health Sciences Authority (HSA) said in a press release on Wednesday (May 27). They include a product called Lung Tan Tsao, which caused adverse effects in a woman who took it, and a product called Candy B+ Coffee Extra Power, which was found to contain more than 50 times the usual daily dose of erectile dysfunction medicine tadalafil. Both products originated overseas and have not been detected for sale in Singapore, according to HSA. The first product, Lung Tan Tsao, caused weight gain and swelling of the face in a woman in her 40s, who got the product from a friend who bought it in Malaysia, said HSA. The product was labelled for the relief of various conditions including eczema, allergies and pain. However, the woman's doctor became suspicious of the product as "it cleared the woman's eczema as rapidly as a prescription medicine would do", said HSA. ubsequent tests revealed antihistamine, chlorpheniramine and a steroid called dexamethasone in the product. "These potent medicinal ingredients can cause serious adverse effects when used without medical supervision," said HSA. Chlorpheniramine is used to relieve allergic reactions such as hives and asthma. Possible adverse effects include nausea, vomiting and diarrhoea. Dexamethasone, a steroid, is usually prescribed for inflammatory conditions and should only be used under strict medical supervision. "Long-term unsupervised use of steroids can cause serious adverse effects including increased blood glucose levels, which may lead to diabetes and Cushing’s syndrome," HSA said. ERECTILE DYSFUNCTION MEDICINE FOUND IN COFFEE PRODUCT The other product, Candy B+ Coffee Extra Power, was brought to HSA's attention after Immigration and Checkpoints Authority officers found 15 boxes of it in a parcel and referred the case to HSA for further investigation. The product, which was labelled a "superfood" and "fountain of youth", claimed to contain known herbal ingredients such as tongkat ali extract, sky fruit extract and maca powder. Its packaging also carried Good Manufacturing Practice and NSF International logos. However when HSA tested the product, it was found to contain more than 50 times the usual daily dose of tadalafil, an erectile dysfunction medicine. Tadalafil can increase the risk of stroke and heart attack if used without medical supervision, said HSA. The misuse of quality certification logos on the product also "aimed to mislead consumers" into thinking that the product is safe and manufactured under high quality standards, said HSA, but there is no way of verifying if these logos are authentic. HSA added that illegal and adulterated products such as Candy B+ Coffee Extra Power can often resurface under a different name or packaging to evade authority checks and trick consumers into buying them. In September 2017, HSA had previously alerted the public to a similar product named Candy B+ Complex, which was also tested to contain tadalafil.  Both products were labelled under the same manufacturer, California Pure. HSA warned it would not hesitate to take action if Lung Tan Tsao and Candy B+ Coffee Extra Power surface on local e-commerce platforms or are found in physical premises. This includes working with website administrators to take down online postings of the products. The authority warned consumers to see a doctor immediately if they have taken Lung Tan Tsao, as discontinuation of steroids without proper medical supervision can cause serious withdrawal symptoms such as fatigue, confusion and low blood pressure. Consumers should stop taking Candy B+ Coffee Extra Power immediately and consult a doctor if they feel unwell or have health concerns. The public should also avoid purchasing health products from unfamiliar sources and be careful when buying such products online or from friends. "You cannot be certain where and how these products were made. They can contain potent ingredients which can seriously harm your health," said HSA. All sellers and suppliers should stop selling Lung Tan Tsao and Candy B+ Coffee Extra Power immediately, said the authority. "It is illegal to sell and supply such products which contain potent medicinal ingredients," it said. If convicted, sellers and suppliers could be jailed for up to two years or fined up to S$10,000, or both. Source: CNA/lk(nc) |
|
#264
|
||||
|
||||
|
Re: Sexual Health News
What is the purpose of pubic hair?
https://www.medicalnewstoday.com/art...ave-pubic-hair Pubic hair serves several purposes, including disease prevention and friction reduction. Whether a person chooses to remove none, all, or some of their pubic hair is a personal choice. Although the media, sexual partners, and societal “norms” can sometimes influence this choice, it should be a personal one. Removing the pubic hair has some risks and potential side effects, but most are mild. Read on to learn more about why humans have pubic hair, the benefits of having pubic hair, and some safe ways to remove it if a person chooses to do so. Purpose Researchers theorize that pubic hair serves three main purposes for the human body. These include: reducing friction during sex preventing bacteria and other microorganisms from transmitting to others maintaining the optimal temperature for the genitals Other theories as to the purpose of pubic hair include trapping pheromones. However, most well-controlled scientific studies have not shown any compelling evidence for this. This ties in with a theory about pubic hair and puberty. Because pubic hair appears during puberty, it is often a physical sign of sexual maturity and may once have served as a visual cue for prospective mates. Benefits The primary benefit of pubic hair is its ability to reduce friction during sexual intercourse. The skin in the area around the genitals is very sensitive. Pubic hair can naturally reduce friction associated with the movements during sexual intercourse and other activities wherein chafing may occur. Pubic hair can also help stop bacteria and other microorganisms from entering the body. Specifically, it can help trap dirt and pathogens that may enter the body through the vagina or penis. According to one 2017 study, pubic hair may help reduce the risk of contracting a sexually transmitted infection (STI). However, additional studies are necessary to prove the effect of pubic hair on preventing STIs. Is there such a thing as too much or too little? Pubic hair is normal, and the amount of hair in the pubic region varies from person to person. There is no standard for the amount, the thickness, or the area that pubic hair will cover. People may notice an extreme variation in hair growth due to hormonal changes. For example, a person may notice excessive pubic hair as a result of polycystic ovary syndrome, while others may notice pubic hair loss due to aging. Is it unhygienic? No, pubic hair is not unhygienic. However, it does trap dirt and sweat, so it can become more pungent than areas of the body that have less hair. Like other areas of the body, pubic hair does require regular cleaning. A person should wash their pubic area whenever they shower or bathe, just as they would other parts of their body. Keeping it clean can help prevent odor. In separate studies, 59% of women and 61% of men stated that they groomed their pubic region for hygienic purposes. However, there is currently no scientific evidence to suggest any health benefits associated with removing pubic hair — other than the removal of pubic lice. Reasons people remove it Pubic hair grooming and removal are fairly common behaviors among adults. In fact, according to one 2015 study, 95% of the participants had removed their pubic hair at least once in the previous 4 weeks. According to the same study, 60% of men and 24% of women were more likely to prefer a “hair-free” partner. People remove their pubic hair for different reasons. Some common reasons include: Personal preference: Some people may prefer the look and feel of having no public hair. Their partner’s preference: There may have been an implied or explicit request to groom or remove the pubic hair. However, pubic hair removal should be an individual’s choice. Increased satisfaction: One 2019 study suggests a correlation between pubic hair removal practices and relationship satisfaction. It also found that women who reported pubic hair removal had enhanced feelings of femininity. Preparation for sexual activity: Hair removal may be particularly beneficial for people who engage in oral sex. Peer or societal pressure: Some people may conform to the way that society believes grooming should occur. Again, however, this should be a personal choice. Risks of removing pubic hair Removing or trimming the pubic hair is a personal choice, though social pressures can sometimes influence this decision. Pubic hair removal is generally safe, but there are some common side effects. These include: itchiness small cuts from razors potential injury, if using a razor or scissors burns from chemical removers rashes infections Pubic grooming injuries are surprisingly common. One 2017 survey found that 25.6% of people who groomed this area sustained injuries during or after hair removal. Also, limited evidence suggests that removing the pubic hair can increase the risk of STIs. However, further research is necessary to determine whether or not removing the pubic hair increases this risk. Best ways to remove pubic hair There are a few methods a person can try to safely remove the pubic hair at home. A person needs to use caution with whichever method they choose to help prevent injury. Some ways to remove hair at home include: Shaving: This removes the hair but may cause chafing, nicks, itchiness, or rashes. Waxing: This removes the hair but is painful and may result in bleeding and irritation. Using chemicals: Depilatory creams can remove the pubic hair, but sensitive skin may burn or react badly to the chemicals. Trimming: A person can use scissors or an electric shaver to trim and maintain pubic hair. Learn more about the best ways to safely remove the pubic hair here. Should a person remove their pubic hair? Whether or not a person removes their pubic hair is a personal decision. Social pressures from peers, partners, or certain media can sometimes influence the decision. However, this should be a personal choice. Some people may prefer to remove their pubic hair because it makes them feel better about themselves. Other people might remove it to feel more attractive to their partner. It is important to discuss this with a partner, however. Ultimately, a person needs to determine how they feel about the decision and do what makes them happiest. Summary Pubic hair plays a role in reducing friction during activities such as sexual intercourse. It also plays a role in preventing dirt and pathogens from entering the genitals. A person can safely remove their pubic hair if they wish to, but they do not need to. Removing pubic hair is generally safe, but it can result in injuries such as burns, nicks, and cuts. A person should use caution no matter how they choose to remove their pubic hair. |
|
#265
|
||||
|
||||
|
Re: Sexual Health News
What you should know about trichomoniasis
https://www.medicalnewstoday.com/articles/307896 Medically reviewed by Carolyn Kay, MD on May 20, 2020 New — Written by Lori Smith, BSN, MSN, CRNP Trichomoniasis is a sexually transmitted infection. A person can pass it on through vaginal, oral, or anal sex. A parasite called Trichomonas vaginalis causes trichomoniasis, or trich, which is highly curable if a person seeks treatment. However, only about 30% of people with trich experience symptoms, according to the Centers for Disease Control and Prevention (CDC). Without treatment, trich can lead to complications. It can affect a pregnancy, and it also appears to increase the risk of getting and passing on HIV. Trichomoniasis is one of the most common sexually transmitted infections (STIs) in the United States, where the CDC estimate that it affects close to 3.7 million people. It is the most common curable STI. Causes and spread T. vaginalis, the parasite that causes trich, can pass from one person to another during sex. A person can transmit it during oral, anal, or vaginal sex or through genital touching. In females, trich is most likely to affect the lower genital tract. In males, it affects the urethra, the tube through which urine passes. Other parts of the body, such as the anus, hands, or mouth, cannot usually become infected. The following people have a higher chance of getting trich: females people with more than one sexual partner those with a history of trich or other STIs people who have unprotected sex As the number of sexual partners that a person has increases, so does their risk of getting trich. Symptoms Symptoms may appear between 5 and 28 days after exposure, or they may appear later or not at all. When symptoms are present, they can affect males and females differently. Minor symptoms include irritation, but someone with a more severe case may have inflammation with discharge. Possible symptoms in females include: frothy, foul-smelling vaginal discharge, which may be clear, white, gray, yellow, or green vaginal discharge with blood genital irritation discomfort during sex or when urinating swelling in the groin frequent urination in rare cases, lower abdominal pain Symptoms in males may include: discharge from the urethra or penis itching in the penis burning sensations after ejaculating or urinating frequent need to urinate pain when urinating Complications Trichomoniasis can lead to several complications, including those below. Problems during pregnancy Experts have linked trichomoniasis with complications during pregnancy, including: preterm birth early rupture of the membrane low birth weight in newborns infertility A woman can sometimes pass on the infection to the newborn during delivery, but this is rare. It is safe to receive treatment with metronidazole during pregnancy. Other problems Trich may increase the risk of reproductive tract infections. At least one study suggests that there may also be a link between trich and human papillomavirus (HPV), the virus that causes cervical cancer. More research is necessary, however, to clarify the association. HIV risk A trich infection can increase the risk of getting HIV and other STIs, especially in females. Scientists believe that this increased risk could be due to: inflammation a reduced immune response changes in the balance of vaginal flora, in females These factors may lower a person’s natural protection from the virus. Tests and diagnosis To diagnose a trichomoniasis infection, a doctor will: carry out a pelvic exam take a sample of vaginal or penile discharge for examination under a microscope take a vaginal swab for a culture test in a laboratory The results of a lab test will come back in about a week. Preparing for the appointment Women should aim to schedule the appointment for a time when they are unlikely to be menstruating. Before the appointment, they should avoid using deodorant on the vulva, as this masks odor and can cause irritation. The doctor may also advise them to avoid vaginal intercourse or inserting any object, including tampons, into the vagina for 24–48 hours beforehand A Pap (smear) test does not check for trich. If a person has a clear Pap test, they may still have trich or another STI. As trich increases the risk of passing on HIV, people with HIV should also have a trich test at least once a year. If the result is positive If the test results are positive, a doctor will prescribe treatment and discuss what to do next. The person will need to: inform all of their sex partners, as they will also need a test take the whole dose or course of treatment to stop the infection from coming back avoid sexual contact until the treatment is complete seek further advice if symptoms remain a few days after finishing a course of antibiotics The doctor may also recommend having tests for other STIs. Treatment Trich is easy to treat in males and females, including during pregnancy. Treatment usually involves taking a single dose of an antibiotic by mouth. A doctor may also prescribe a vaginal suppository or a cream to apply topically. Antibiotic medications that kill parasites include metronidazole (Flagyl) and tinidazole (Tindamax). People should not consume alcohol while taking metronidazole, as there may be an adverse reaction, which can lead to abdominal cramps, nausea, headaches, and flushing. If symptoms continue after taking the treatment, a person should go back to see their doctor again. Breastfeeding after treatment People should not take tinidazole while breastfeeding. Metronidazole is safe to use, but a doctor may suggest waiting 12–24 hours after taking it before breastfeeding. Prevention To prevent infection or reinfection, any sexual partners should also receive treatment. Ways of preventing the risk of infection or reinfection include: limiting the number of sexual partners avoiding sex for 7–10 days after treatment for trich not using a douche, as this can affect the healthy bacteria in the vagina limiting or avoiding the use of recreational drugs and alcohol, as these increase the risk of unsafe sex using a condom for protection during sex A condom can prevent transmission to some extent, but it is not fully reliable because the parasite can pass from person to person on areas of the body that it does not cover. Anyone who has symptoms or thinks that they have been exposed to trich should speak to a doctor. Takeaway Trichomoniasis is a sexually transmitted infection. It spreads easily and can lead to complications, but effective treatment is available. Treatment can prevent complications and stop trich from spreading to another person. |
|
#266
|
||||
|
||||
|
Re: Sexual Health News
What to expect during menopause
https://www.medicalnewstoday.com/articles/155651 Menopause is a transition into a new phase of life. It begins when the menstrual cycle finishes. Menopause is not a health problem, and some experience it as a time of liberation. However, hormonal changes and other factors involved can cause discomfort. Menopause usually starts between the ages of 40 and 58 years in developed countries, where the average age is 51 years. For some, it will occur earlier due to a medical condition or treatment, such as the removal of the ovaries. Around the time of menopause, many females experience physical symptoms such as hot flashes, night sweats, vaginal dryness, and a reduced sex drive. It can also lead to anxiety, changes in mood, and a reduced sex drive. These symptoms may start before menstruation ends, and they can last for several years. The impact on a person’s quality of life can range from mild to severe. However, there are ways of managing these symptoms. Each person will experience menopause differently. Many have full, active lives throughout the transition and afterward, and some feel relieved by no longer having to deal with menstruation or birth control. Maintaining a healthful diet and getting regular exercise can help a person feel better and boost their overall health in the long term. For those who experience menopause symptoms, treatments and support are available. In this article, find out more about what to expect during menopause. What is menopause? Menopause is the stage of life that follows the end of the menstrual cycles. Each person may experience menopause differently. It can last for several years, and there are three stages: Perimenopause is the transitional time that starts before menopause and includes the 12 months that follow a person’s last period. Menopause starts either 12 months after the last period or when menstruation has stopped for a clinical reason, such as the removal of the ovaries. Postmenopause refers to the years after menopause, although it can be difficult to know when menopause finished and postmenopause starts. How long do menopause symptoms last? Find out here. Signs and symptoms Around menopause, various physical and mental changes can occur, causing symptoms. Some of these start before menopause, and some continue after it. The changes involved in perimenopause and menopause include: Lower fertility As a female approaches the end of the reproductive stage, but before menopause begins, estrogen levels start to fall. This reduces the chances of becoming pregnant. Irregular menstruation The first sign that menopause is approaching is usually periods occurring less regularly. They may come more or less frequently than usual, and they may be heavier or lighter. Anyone who has concerns about menstrual changes should see a doctor, as these changes can also indicate pregnancy or some health issues. Is it normal to have brown spotting after menopause? Vaginal dryness and discomfort Vaginal dryness, itching, and discomfort may start during perimenopause and continue into menopause. A person with any of these symptoms may experience chafing and discomfort during vaginal sex. Also, if the skin breaks, this can increase the risk of infection. Atrophic vaginitis, which involves thinning, drying, and inflammation of the vaginal wall, can sometimes occur during menopause. Various moisturizers, lubricants, and medications can relieve vaginal dryness and associated issues. Hot flashes Hot flashes are common around the time of menopause. They cause a person to feel a sudden sensation of heat in the upper body. The sensation may start in the face, neck, or chest and progress upward or downward. A hot flash can also cause: sweating red patches to form on the skin Some people experience night sweats and cold flashes, or chills, in addition to or instead of hot flashes. Hot flashes usually occur in the first year after menstruation ends, but they can continue for up to 14 years after menopause. Sleep disturbances Sleep problems can arise during menopause, and they may stem from: anxiety night sweats an increased need to urinate Getting plenty of exercise and avoiding heavy meals before bedtime can help with managing these issues, but if they persist, contact a healthcare provider. Emotional changes Depression, anxiety, and low mood are common during menopause. It is not unusual to experience times of irritability and crying spells. Hormonal changes and sleep disturbances can contribute to these issues. Also, a person’s feelings about menopause may come into play. For example, distress about low libido or the end of fertility can contribute to depression during menopause. While feelings of sadness, irritability, and tiredness are common during menopause, they do not necessarily indicate depression. However, anyone who experiences a low mood for 2 weeks or longer should see a doctor, who will be able to advise about the best course of action. Anyone who has concerns about sleep or any changes related to menopause should contact a healthcare provider. An article published in 2018 suggests that there may, in some cases, be a link between menopause and suicide. Anyone who is thinking about suicide should seek help from a counselor or health professional. There are also anonymous hotlines available. Trouble focusing and learning In the lead-up to menopause two-thirds of women may have difficulty with concentration and memory. Keeping physically and mentally active, following a healthful diet, and maintaining an active social life can help with these issues. For example, some people benefit from finding a new hobby or joining a club or a local activity. Physical changes Various physical changes can develop around the time of menopause. People may experience: a buildup of fat around the abdomen weight gain changes in hair color, texture, and volume breast reduction and tenderness urinary incontinence However, the link between these changes and menopause is not always clear. Some may occur independently at the same time as the transition, and age and lifestyle can also play a role. Increased risk of some health conditions After menopause, the risk of certain health issues appears to increase. Menopause does not cause these conditions, but the hormonal changes involved may play some role. Osteoporosis: This is a long-term condition in which bone strength and density decrease. A doctor may recommend taking vitamin D supplements and eating more calcium-rich foods to maintain bone strength. Find out more about osteoporosis treatments. Cardiovascular disease: The American Heart Association (AHA) note that, while a decline in estrogen due to menopause may increase the risk of cardiovascular disease, taking hormone therapy will not reduce this risk. Breast cancer: Some types of breast cancer are more likely to develop after menopause. Menopause does not cause breast cancer, but hormonal changes involved appear to increase the risk. Skin changes can also occur around the time of menopause LGBTQIA+ and menopause Most information about menopause describes the experiences of cisgender, heterosexual women. However, menopause can affect anyone who is born with ovaries. A person who transitions to male but who retains their ovaries may experience menopause when their ovaries stop producing eggs. If a person starts taking supplementary testosterone as part of their transition, they may experience menopause symptoms then. Also, menopause symptoms can develop when a person undergoes surgery to remove their ovaries. When transitioning involves any of these experiences, the symptoms of menopause will be the same as those of cisgender women. However, transgender people can face additional difficulties, depending on the attitude of their medical team. It is essential that transgender people have access to healthcare providers who understand their needs and can address them effectively. Treatment Menopause is not a health problem but a natural transition. However, it can involve unwanted physical and mental changes. Anyone who has concerns about these changes should seek medical advice. A doctor may recommend one or more of the following: Hormone therapy This treatment helps balance the body’s hormone levels by providing supplemental estrogen and a synthetic version of the hormone progesterone. Hormone therapy comes in various forms, including skin patches and topical creams. It can help reduce the occurrence of hot flashes and other menopause symptoms. However, using it may increase the risk of developing certain diseases and health conditions. A person should not use hormone therapy if they have risk factors for the following health problems, or if they have a personal or family history of these issues: heart disease blood clots high levels of triglycerides in the blood gallbladder disease liver disease stroke breast cancer It is important to discuss the possible benefits and risks of hormone therapy with a doctor before deciding to use it. Other treatments A person may find that the following can also help relieve symptoms: over-the-counter gels and other products for vaginal dryness prescription pills, creams, and rings for vaginal dryness low-dose hormonal birth control pills for hot flashes, vaginal dryness, and mood changes low-dose antidepressants for hot flashes, even among people who do not have depression Lifestyle tips Tips for managing the challenges of menopause include: getting regular exercise practicing relaxation and deep breathing exercises having a healthful diet that includes plenty of fresh fruits, vegetables, and whole grains quitting smoking and avoiding secondhand smoke limiting the intake of alcohol seeking counseling for anxiety, mood changes, and relationship concerns establishing good sleeping habits and getting plenty of rest doing Kegel exercises to strengthen the pelvic floor talking to friends and family about the experience of menopause exploring new ways of enjoying intimacy with a partner joining a club, volunteering, or taking up a new hobby Can I use coconut oil for vaginal dryness? Keeping an active sex life Menopause can reduce a person’s sex drive and lead to vaginal dryness, but it also removes the need for birth control. For some, this can make sex more enjoyable. Having sex often can increase vaginal blood flow and help keep the tissues healthy. Some tips for maintaining sexual health and activity during menopause include: staying physically active avoiding tobacco products, recreational drugs, and alcohol taking the time to become aroused, which will improve lubrication doing Kegel exercises to strengthen the pelvic floor not using any strong soaps around the vagina, as these can worsen irritation Also, menopause symptoms lead some people to find satisfying forms of sex that do not involve the vagina as much or at all. It is worth remembering that, while a woman cannot become pregnant once menopause starts, it is still important to use barrier protection during penetrative sex to protect against sexually transmitted infections. Often, sexual partners will be getting older — and may be experiencing menopause — at the same time. They, too, may be feeling a drop in sex drive. Opening up about any concerns can help both partners feel better and explore new forms of intimacy. Causes Menopause is a stage in life, not an illness. Most women experience natural menopause during midlife. However, surgery and other factors can cause menopause to start earlier. Natural menopause A female’s reproductive years last from puberty to menopause — from one natural transition to another. Toward menopause, the levels of the hormones estrogen and progesterone in the body fall because they are no longer necessary to support reproduction. These changes trigger menopause. Surgery and treatment If a person undergoes surgery to remove their ovaries, they will experience menopause. If this happens before middle age, doctors may refer to it as “early menopause.” A doctor may recommend hormone therapy to reduce some symptoms, but as always, it is important to discuss the risks as well as the potential benefits of this treatment. Some treatments, such as chemotherapy and radiotherapy, can cause the ovaries to stop working either temporarily or permanently. The likelihood of this happening depends on the person’s age and the type and location of the treatment. A person who experiences menopause because of a clinical treatment will experience the same symptoms as a person who experiences natural menopause. However, the symptoms may appear more abruptly, because the physical change is more sudden. A person may also experience sadness or depression about an early loss of fertility. Some people decide to freeze eggs or pursue other options for having children later in life before undergoing this type of treatment. Counseling is often available. It is also important to discuss related health effects with a doctor, as people who experience menopause early may have a higher risk of developing heart disease and osteoporosis. Premature menopause Some people experience menopause earlier than others for reasons other than medical interventions. Doctors consider menopause to be “premature” if it develops before the age of 40 and “early” if it starts between the ages of 40 and 45. Early menopause naturally occurs in around 5% of females. Sometimes, menopause develops early if a person has: a genetic condition that affects the chromosomes, such as Turner’s syndrome an autoimmune disease in rare cases, an infection, such as tuberculosis, malaria, or mumps Anyone who experiences changes in menstrual patterns before the age of 45 should see a doctor. Diagnosis Menopause is not an illness, but many people benefit from seeing their doctors when menstruation ends. A doctor can often confirm whether the reason for this change is perimenopause or menopause by asking some questions. They may also test hormone levels and perform other analyses of the blood and urine to rule out health issues. No tests, however, can conclusively indicate that menopause has begun. People can check their hormone levels at home with testing kits, some of which are available for purchase online. Summary For many people, menopause is not the only transition that occurs during middle age. Changes in relationships and work or home life — such as children moving away — can also have a significant impact. When more than one of these changes occurs in a short period, it can feel overwhelming. However, many people live active, healthy lives throughout menopause and for many decades afterward, and midlife can often be the start of a new chapter. |
|
#267
|
||||
|
||||
|
Re: Sexual Health News
Man fined for having unregistered health products including pills and more than 40,000 condoms for sale
https://www.channelnewsasia.com/news...ndoms-12977096 SINGAPORE: A man was fined S$32,500 on Thursday (Jul 30) for having unregistered health products including more than 40,000 condoms, contraceptive pills and medical devices for sale. If he cannot pay the fine, he will have to serve 130 days' jail. Song Bowen, 27, pleaded guilty to 13 counts of supplying unregistered health products under the Health Products Act, with another 25 charges taken into consideration. The case was uncovered after Song fell for a set-up, meeting a police officer at a void deck in Yishun to sell him emergency contraceptive pills. The pills are unregistered health products containing Levonorgestrel, an active ingredient present in prescription-only medicines. It is used as an emergency contraceptive to prevent pregnancy after unprotected sex, and no more than four tablets can be taken per month, said the Health Sciences Authority (HSA) prosecutor. The officer bought a tablet for S$20 and later sent him a message asking to buy more of the tablets and to see other brands of contraceptive tablets. Song took three types of contraceptive pills and met the officer again outside Song's Yishun flat. However, the officer identified himself as a police officer, arrested Song and seized the tablets. HSA officers raided Song's flat that day and found an assortment of unregistered health products including thousands of condoms and "therapeutic products". The seized items included multiple brands of condoms, with between 3,980 and 7,700 pieces per brand. Song admitted that he intended to sell each box of 10 condoms for S$10. The defence asked for community-based sentences, adding that Song had not made profits from the condoms at the point of his arrest. At this, the judge asked the prosecutor how many condoms in total were seized. When told it was 40,000, he said: "40,000! What sort of inference is the court supposed to draw, with the fact that he has 40,000 condoms in his possession?" He said that Song had possessed the items for the purpose of selling them. Song is studying part-time at a university and works full-time at an engineering company, his lawyer said. He has to remit money to China for his family and has to pay tuition fees and rental, said the lawyer, asking for the fine to be paid in instalments. The judge granted his request to pay in instalments by May next year. The seized condoms and pills were forfeited for disposal. For each charge of supplying an unregistered health product, Song could have been jailed for up to two years, fined up to S$50,000, or both. |
|
#268
|
||||
|
||||
|
Re: Sexual Health News
HSA raises alert on products containing banned substance sibutramine, erectile dysfunction medicine
https://www.channelnewsasia.com/news...lafil-12994792  SINGAPORE: The Health Sciences Authority (HSA) on Thursday (Aug 6) issued an alert about two slimming products found to contain a banned substance that could pose serious health risks. A medicinal ingredient used to treat erectile dysfunction was also found in another product sold online as candy, said the authority in a media release. HSA was alerted to the product Coco Curv by a consumer who had bought it in Malaysia. She suspected that the product could be harmful and reported it to the authority. Marketed online as a slimming product, Coco Curv claimed to "burn fat and calories", "boost energy and metabolism", as well as "control carbohydrate craving".  During investigations into Coco Curv, HSA came across another slimming product online called Choco Fit. Tests revealed that both products contained the banned substance sibutramine. The drug used to be a prescription medicine for weight loss, but has been banned in Singapore since 2010 due to an increased risk of heart attacks and strokes. HSA said other serious adverse effects reported by consumers who took products with sibutramine include rapid heartbeat, insomnia, and suicidal thoughts. 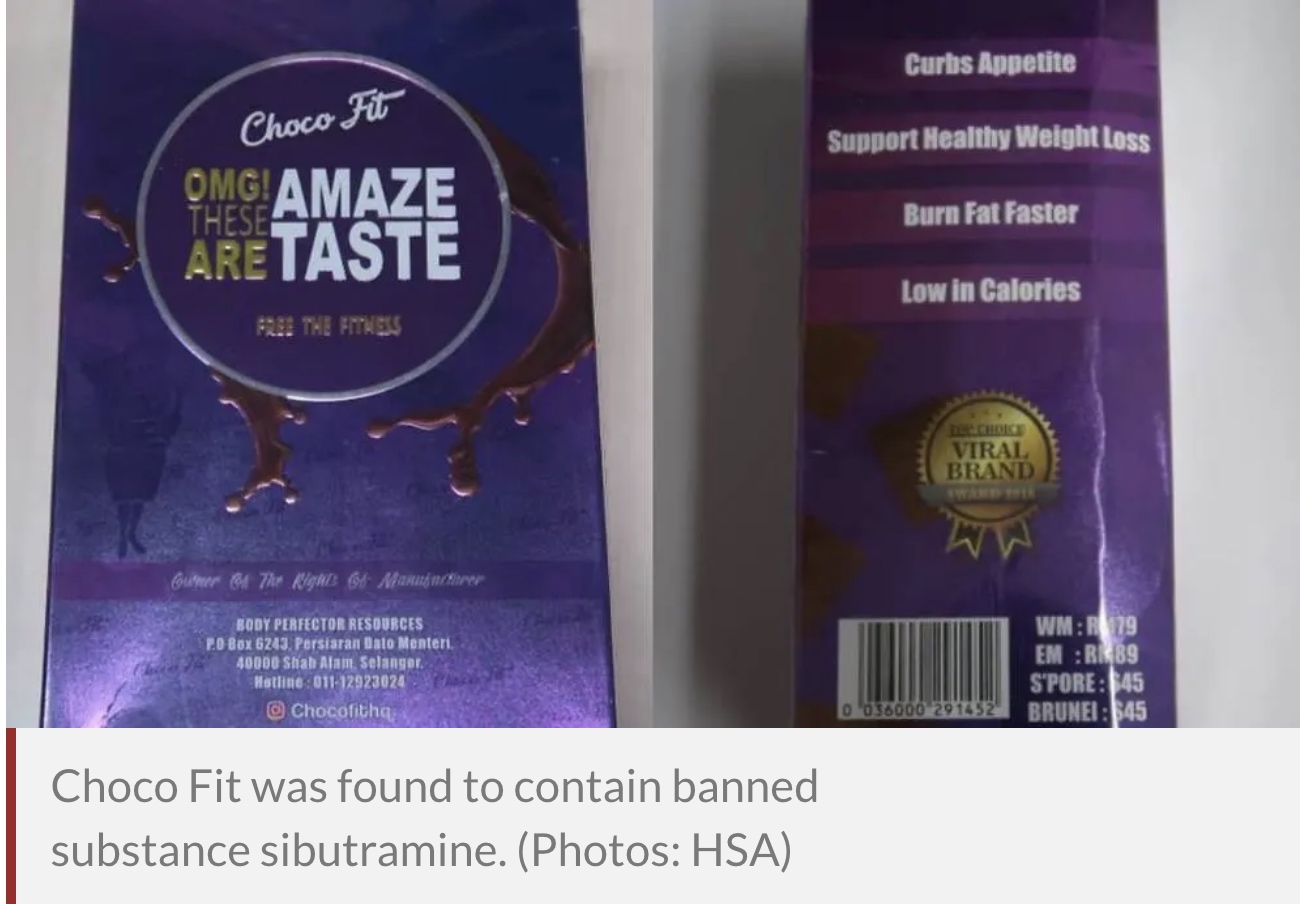 ERECTILE DYSFUNCTION MEDICINE FOUND IN HAMER CANDY In the release, HSA said it was also alerted by a consumer to another product Hamer Candy containing a potent ingredient. The product, packaged as a candy, was found to have nortadalafil, which is chemically related to tadalafil. 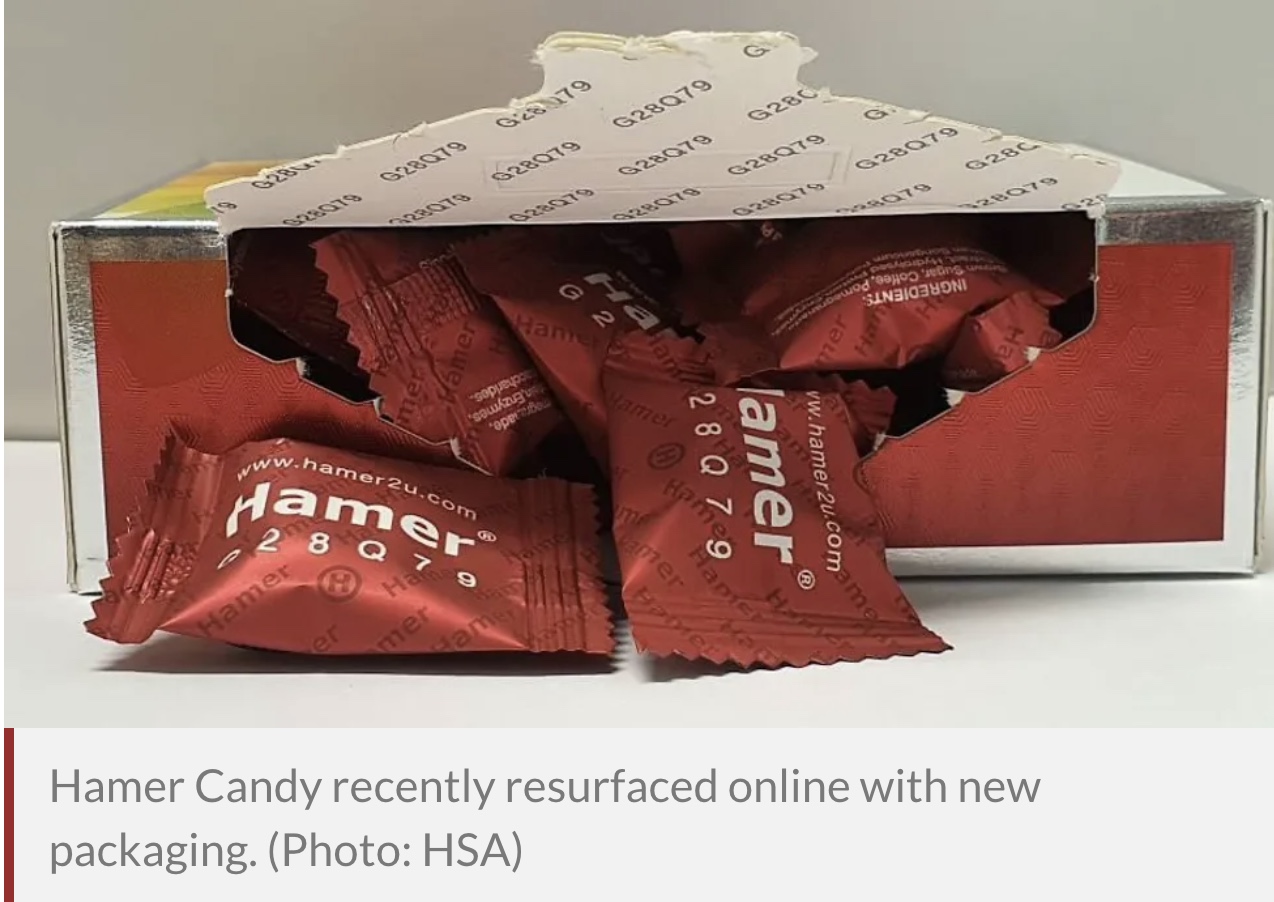 Tadalafil is a prescription medicine used to treat male erectile dysfunction, said HSA. Inappropriate use of tadalafil without medical supervision may also cause priapism, which is a painful and prolonged erection. Tadalafil can also pose serious risks to certain patients, including those with heart-related problems. It should not be used by patients who are on heart medications such as nitrates as it can cause potentially life-threatening low blood pressure. HSA added that the use of nortadalafil may lead to increased risk of serious adverse effects including low blood pressure, strokes and heart attacks. Both Hamer Candy and Choco Fit had previously been alerted to members of the public in 2018 and 2019 respectively, said HSA. Online postings of these products were also taken down. However, they have recently resurfaced online with new packaging, said HSA. This is "a common tactic undertaken by unscrupulous manufacturers in an attempt to evade detection and entice consumers". All three products were sold on local online platforms including Shopee, Qoo10, as well as on Facebook and Instagram. HSA said it has issued warnings to the sellers and directed the respective website administrators to take down the affected listings. Source: CNA/ad(rw) |
|
#269
|
||||
|
||||
|
Re: Sexual Health News
What are the side effects of not releasing sperm?
https://www.medicalnewstoday.com/art...eleasing-sperm Medically reviewed by Joseph Brito III, MD — Written by Aaron Kandola on November 16, 2020 Not releasing sperm is usually harmless, but it depends on the cause. Some forms of sexual dysfunction can cause problems releasing sperm and lead to infertility. Keep reading to learn more about the importance of ejaculating, possible issues, and some treatment options. Why is it important to ejaculate? In most cases, it is not harmful for a person to ejaculate, but it depends on the cause. Ejaculation refers to the expulsion of semen from the body. Typically, sexual stimulation causes the central nervous system to build arousal to the point of orgasm. During this process, sperm from the testicles travel through the epididymis and into the vas deferens. From here, it enters the urethra through the prostate’s ejaculatory ducts, mixing with seminal fluid, which comes from the seminal vesicles, and prostate secretions. The contraction of the pelvic muscles expels this fluid, now called semen, from the tip of the penis. Several factors can prevent stimulation leading to ejaculation. Ejaculation usually occurs with an orgasm, but not always. The causes of preventing ejaculation can be intentional or unintentional. Intentionally preventing ejaculation Some people choose to delay ejaculation, such as during edging. Edging is when a person builds sexual stimulation almost to the point of orgasm but stops just before it occurs. Edging is unlikely to cause health problems. In rare cases, it can cause epididymal hypertension, or “blue balls.” Other people intentionally prevent ejaculation entirely, such as those practicing Taoism. Sexual dysfunction In other cases, medical conditions can prevent ejaculation. For example, nerve damage can cause delayed ejaculation. Males with delayed ejaculation experience difficulty or inability to ejaculate in a reasonable time. Anejaculation is where people are completely unable to ejaculate semen. People with this condition can still produce sperm and experience orgasms — however, they cannot ejaculate. Anejaculation has a range of triggers, from pelvic injuries to acquiring infections. The condition can lead to infertility without treatment. Retrograde ejaculation is where some or all of the sperm enters the bladder instead of out of the penis. The condition can also lead to infertility, but further issues are unlikely. Retrograde ejaculation is sometimes due to side effects from certain medications, such as tamsulosin. It is a harmless condition but may cause concern in some people. Side effects of not ejaculating The side effects of not ejaculating depend on the cause and the person. People who choose not to ejaculate are unlikely to experience harmful side effects. The body breaks down unused sperm, which does not build up to trigger further problems. Over time, not ejaculating can trigger psychological problems. For example, people with sexual dysfunctions that affect their ability to ejaculate may experience distress or embarrassment. It can also lead to relationship problems. For example, partners may become frustrated with a person with sexual dysfunction. These psychological problems could lead to mental health conditions, such as depression or anxiety disorders. Treatment Not everyone needs treatment for not ejaculating. For example, people who practice edging choose to delay ejaculation. There are several treatments for people with sexual dysfunctions that prevent ejaculation, depending on their cause. Many triggers are psychological, and people may benefit from psychotherapy or counseling. These sessions may involve the individual alone or with their partner. Other causes are physical. For example, people with an infection can experience anejaculation or retrograde ejaculation. In these cases, a doctor may prescribe antibiotics or antiviral medications. Some medications or drugs can also cause sexual dysfunction as a side effect. For example, antidepressant use or excessive alcohol consumption could cause delayed ejaculation. Changing medications and reducing alcohol consumption can help in these situations. In addition, certain medical procedures, such as prostate surgery, can lead to retrograde ejaculation. Tips for ejaculation People who are unable to ejaculate due to sexual dysfunction should talk to a doctor about treatment. Some may also benefit from sex therapy. Sex therapists use a variety of techniques to help people with sexual dysfunction, including psychotherapy and mindfulness. Other general tips that can help include: avoiding excessive alcohol consumption before intercourse being aware of medication side effects, which may include sexual dysfunction talking to a partner about the problem practicing stress management techniques seeking help from a professional for mental health problems When to see a doctor It is normal to have problems ejaculating from time to time. People who can ejaculate occasionally are unlikely to need medical treatment. Those who intentionally avoid ejaculation also do not need further healthcare. It is worth seeing a doctor if the problem is due to sexual dysfunction. For example, people who regularly experience issues or are unable to ejaculate at all should consult a healthcare professional. Many causes of sexual dysfunction are psychological. Talking to a partner about these problems is one way to address these issues. A mental health professional can also help. Summary Not ejaculating is rarely harmful, but it depends on the cause. Some people choose not to ejaculate, such as those practicing edging. Others cannot ejaculate due to sexual dysfunction. People should see a doctor if they consistently experience issues with ejaculation. Healthcare professionals can discuss possible treatment options. |
|
#270
|
|||
|
|||
|
Re: Sexual Health News
thank you all for sharing this well written information helpful for all online readers. Keep sharing
|
| Advert Space Available |
 |
| Bookmarks |
| Thread Tools | |
|
|
 t Similar Threads
t Similar Threads
|
||||
| Thread | Thread Starter | Forum | Replies | Last Post |
| Non sexual health question | sicknasty | Sexual Health Issues | 7 | 10-01-2015 05:45 AM |
| Sexual Health Issues | Whybother | Sexual Health Issues | 2 | 24-04-2013 07:02 AM |
| DSC Sexual Health Screening | Huluman | Sexual Health Issues | 3 | 23-11-2008 08:57 PM |
| Sexual Health & Well Being | MrDevil | Sexual Health Issues | 10 | 29-03-2004 09:36 AM |
| sexual health mentor | boyrusty2000 | Sexual Health Issues | 31 | 06-08-2003 11:10 PM |