
 |
|
#241
|
|||
|
|||
|
Re: Sexual Health News
|
|
#242
|
|||
|
|||
|
Re: Sexual Health News
Good news. The above CDC website says that PrEP, a new medicine, can be eaten before sex. Then heterosexual or gay couples can have sex without condoms. They will not get HIV. PrEP is basically anti retroviral HIV drugs that can be eaten before sex. Another advance against HIV and AIDS. HIV is now like a chronic medical condition like being a Hepatitis carrier. We must remove the stigma against AIDS.
|
|
#243
|
||||
|
||||
|
Re: Sexual Health News
just afew correction....PrEP isnt new and it isnt just something to pop just before sex.....
it is a preventive measure and not 100% guarantee against getting HIV.. and it also uses the same drug combo as PEP.. https://sbf.today/showpost.p...&postcount=857 Quote:
|
|
#244
|
||||
|
||||
|
Re: Sexual Health News
everyone should read this..
Crisis Looms in Antibiotics as Drug Makers Go Bankrupt By Andrew Jacobs Published Dec. 25, 2019 Updated Dec. 26, 2019 https://www.nytimes.com/2019/12/25/h...esistance.html Crisis Looms in Antibiotics as Drug Makers Go Bankrupt First Big Pharma fled the field, and now start-ups are going belly up, threatening to stifle the development of new drugs. At a time when germs are growing more resistant to common antibiotics, many companies that are developing new versions of the drugs are hemorrhaging money and going out of business, gravely undermining efforts to contain the spread of deadly, drug-resistant bacteria. Antibiotic start-ups like Achaogen and Aradigm have gone belly up in recent months, pharmaceutical behemoths like Novartis and Allergan have abandoned the sector and many of the remaining American antibiotic companies are teetering toward insolvency. One of the biggest developers of antibiotics, Melinta Therapeutics, recently warned regulators it was running out of cash. Experts say the grim financial outlook for the few companies still committed to antibiotic research is driving away investors and threatening to strangle the development of new lifesaving drugs at a time when they are urgently needed. “This is a crisis that should alarm everyone,” said Dr. Helen Boucher, an infectious disease specialist at Tufts Medical Center and a member of the Presidential Advisory Council on Combating Antibiotic-Resistant Bacteria. The problem is straightforward: The companies that have invested billions to develop the drugs have not found a way to make money selling them. Most antibiotics are prescribed for just days or weeks — unlike medicines for chronic conditions like diabetes or rheumatoid arthritis that have been blockbusters — and many hospitals have been unwilling to pay high prices for the new therapies. Political gridlock in Congress has thwarted legislative efforts to address the problem. The challenges facing antibiotic makers come at time when many of the drugs designed to vanquish infections are becoming ineffective against bacteria and fungi, as overuse of the decades-old drugs has spurred them to develop defenses against the medicines. Drug-resistant infections now kill 35,000 people in the United States each year and sicken 2.8 million, according a report from the Centers for Disease Control and Prevention released last month. Without new therapies, the United Nations says the global death toll could soar to 10 million by 2050. The newest antibiotics have proved effective at tackling some of the most stubborn and deadly germs, including anthrax, bacterial pneumonia, E. coli and multi-drug-resistant skin infections. The experience of the biotech company Achaogen is a case in point. It spent 15 years and a billion dollars to win Food and Drug Administration approval for Zemdri, a drug for hard-to-treat urinary tract infections. In July, the World Health Organization added Zemdri to its list of essential new medicines. By then, however, there was no one left at Achaogen to celebrate. This past spring, with its stock price hovering near zero and executives unable to raise the hundreds of millions of dollars needed to market the drug and do additional clinical studies, the company sold off lab equipment and fired its remaining scientists. In April, the company declared bankruptcy. Public health experts say the crisis calls for government intervention. Among the ideas that have wide backing are increased reimbursements for new antibiotics, federal funding to stockpile drugs effective against resistant germs and financial incentives that would offer much needed aid to start-ups and lure back the pharmaceutical giants. Despite bipartisan support, legislation aimed at addressing the problem has languished in Congress. “If this doesn’t get fixed in the next six to 12 months, the last of the Mohicans will go broke and investors won’t return to the market for another decade or two,” said Chen Yu, a health care venture capitalist who has invested in the field. The industry faces another challenge: After years of being bombarded with warnings against profligate use of antibiotics, doctors have become reluctant to prescribe the newest medications, limiting the ability of companies to recoup the investment spent to discover the compounds and win regulatory approval. And in their drive to save money, many hospital pharmacies will dispense cheaper generics even when a newer drug is far superior. “You’d never tell a cancer patient, ‘Why don’t you try a 1950s drug first and if doesn’t work, we’ll move on to one from the 1980s,’” said Kevin Outterson, the executive director of CARB-X, a government-funded nonprofit that provides grants to companies working on antimicrobial resistance. “We do this with antibiotics and it’s really having an adverse effect on patients and the marketplace.” Many of the new drugs are not cheap, at least when compared to older generics that can cost a few dollars a pill. A typical course of Xerava, a newly approved antibiotic that targets multi-drug-resistant infections, can cost as much as $2,000. “Unlike expensive new cancer drugs that extend survival by three-to-six months, antibiotics like ours truly save a patient’s life,” said Larry Edwards, chief executive of the company that makes Xerava, Tetraphase Pharmaceuticals. “It’s frustrating.” Tetraphase, based in Watertown, Mass., has struggled to get hospitals to embrace Xerava, which took more than a decade to discover and bring to market, even though the drug can vanquish resistant germs like MRSA and CRE, a group of resistant bacteria that kills 13,000 people a year. Tetraphase’s stock price has been hovering around $2, down from nearly $40 a year ago. To trim costs, Mr. Edwards recently shuttered the company’s labs, laid off some 40 scientists and scuttled plans to move forward on three other promising antibiotics. For Melinta Therapeutics based in Morristown, N.J., the future is even grimmer. Last month, the company’s stock price dropped 45 percent after executives issued a warning about the company’s long-term prospects. Melinta makes four antibiotics, including Baxdela, which recently received F.D.A. approval to treat the kind of drug-resistant pneumonia that often kills hospitalized patients. Jennifer Sanfilippo, Melinta’s interim chief executive, said she was hoping a sale or merger would buy the company more time to raise awareness about the antibiotics’ value among hospital pharmacists and increase sales. “These drugs are my babies, and they are so urgently needed,” she said. Coming up with new compounds is no easy feat. Only two new classes of antibiotics have been introduced in the last 20 years — most new drugs are variations on existing ones — and the diminishing financial returns have driven most companies from the market. In the 1980s, there were 18 major pharmaceutical companies developing new antibiotics; today there are three. “The science is hard, really hard,” said Dr. David Shlaes, a former vice president at Wyeth Pharmaceuticals and a board member of the Global Antibiotic Research and Development Partnership, a nonprofit advocacy organization. “And reducing the number of people who work on it by abandoning antibiotic R & D is not going to get us anywhere.” A new antibiotic can cost $2.6 billion to develop, he said, and the biggest part of that cost is the failures along the way. Some of the sector’s biggest players have coalesced around a raft of interventions and incentives that would treat antibiotics as a global good. They include extending the exclusivity for new antibiotics to give companies more time to earn back their investments and creating a program to buy and store critical antibiotics much the way the federal government stockpiles emergency medication for possible pandemics or bioterror threats like anthrax and smallpox. The DISARM Act, a bill introduced in Congress this year, would direct Medicare to reimburse hospitals for new and critically important antibiotics. The bill has bipartisan support but has yet to advance. One of its sponsors, Senator Bob Casey, Democrat of Pennsylvania, said some of the reluctance to push it forward stemmed from the political sensitivity over soaring prescription drug prices. “There is some institutional resistance to any legislation that provides financial incentives to drug companies,” he said. Washington has not entirely been sitting on its hands. Over the past decade, the Biomedical Advanced Research and Development Authority, or BARDA, a federal effort to counter chemical, nuclear and other public health threats, has invested a billion dollars in companies developing promising antimicrobial drugs and diagnostics that can help address antibiotic resistance. “If we don’t have drugs to combat these multi-drug-resistant organisms, then we’re not doing our job to keep Americans safe,” Rick A. Bright, the director of the agency, said. Dr. Bright has had a firsthand experience with the problem. Two years ago, his thumb became infected after he nicked it while gardening in his backyard. The antibiotic he was prescribed had no effect, nor did six others he was given at the hospital. It turned out he had MRSA. The infection spread, and doctors scheduled surgery to amputate the thumb. His doctor prescribed one last antibiotic but only after complaining about its cost and warning that Dr. Bright’s insurance might not cover it. Within hours, the infection began to improve and the amputation was canceled. “If I had gotten the right drug on Day 1, I would have never had to go to the emergency room,” he said. Achaogen and its 300 employees had held out hope for government intervention, especially given that the company had received $124 million from BARDA to develop Zemdri. As recently as two years ago, the company had a market capitalization of more than $1 billion and Zemdri was so promising that it became the first antibiotic the F.D.A. designated as a breakthrough therapy, expediting the approval process. Dr. Ryan Cirz, one of Achaogen’s founders and the vice president for research, recalled the days when venture capitalists took a shine to the company and investors snapped up its stock. “It wasn’t hype,” Dr. Cirz, a microbiologist, said. “This was about saving lives.” In June, investors at the bankruptcy sale bought out the company’s lab equipment and the rights to Zemdri for a pittance: $16 million. (The buyer, the generic-drug maker Cipla USA, has continued to manufacture the drug.) Many of Achaogen’s scientists have since found research jobs in more lucrative fields like oncology. Dr. Cirz lost his life savings, but he said he had bigger concerns. Without effective antibiotics, many common medical procedures could one day become life-threatening. “This is a problem that can be solved, it’s not that complicated,” he said. “We can deal with the problem now, or we can just sit here and wait until greater numbers of people start dying. That would be a tragedy.” Matt Richtel contributed reporting. |
|
#245
|
||||
|
||||
|
Re: Sexual Health News
Antibiotics maker Melinta files for Chapter 11 bankruptcy
Reporting by Dania Nadeem in Bengaluru; Editing by Anil D'Silva https://www.reuters.com/article/us-m...-idUSKBN1YV1AT (Reuters) - Melinta Therapeutics Inc said on Friday it had filed for bankruptcy protection, becoming the latest casualty of a persistent cash burn in the antibiotic industry. The drugmaker, which has four antibiotics on the market, warned that it was running out of cash last month. Global health officials have repeatedly warned about the rise of bacteria and other microbes that are resistant to most drugs due to their overuse, prompting health agencies to push for newer versions of antibiotics. However, antibiotics are relatively cheap and are more effective the less they are used, making profitability hard to achieve. Larger drugmakers, including AstraZeneca Plc, Novartis and Sanofi SA, have stopped developing antibiotics, while smaller players such as Achaogen Inc have filed for bankruptcy. Melinta, which filed for Chapter 11 in the U.S. Bankruptcy Court for the District of Delaware, said lenders would acquire the company by exchanging $140 million of claims under their credit facility for all of the company’s equity. The company’s shares were down 53% at 70 cents on Friday. They are down 62% for the year through Thursday close. |
|
#246
|
||||
|
||||
|
Re: Sexual Health News
What causes sores on the penis?
https://www.medicalnewstoday.com/articles/326583.php A sore is a painful bump or wound. Sores can appear on any part of the skin, including on the penis. Penis sores often result from a sexually transmitted infection or a skin condition. While some penis sores will clear up on their own, many require treatment to prevent symptoms from getting worse, complications, and transmission to others. In this article, we list 12 potential causes of penis sores and the treatments available for each one. 1. Genital herpes Genital herpes is a sexually transmitted infection (STI) that passes from one person to another during sexual activity. In the United States, more than 1 in every 6 people aged 14–49 have genital herpes. The herpes simplex virus causes genital herpes. Its symptoms can include painful, itchy, fluid-filled, blistering sores on the penis and other parts of the genitals. When these blisters burst, they can leave scars. Treatment There is no cure for herpes, but antiviral medications can help prevent or treat outbreaks. Individuals should avoid sexual activity until the sores go away. People should also refrain from touching the sores, as this may cause them to spread the virus to other areas.  2. Genital warts Genital warts are another type of viral STI, caused by the human papillomavirus. They appear on the penis as small, bumpy, sometimes stalky, cauliflower-like growths. Genital warts can cause itching and discomfort. Approximately 1% of sexually active people in the U.S. have genital warts at any given time. Treatment If the warts do not cause pain and discomfort, then no treatment is necessary. For up to 1 in 3 people with the condition, the warts will go away on their own within 2 years. To remove the warts, a doctor can freeze them off, perform laser surgery, or prescribe a topical medication to destroy the warts. These treatments do not kill the virus that causes the warts, however, so they may return in the future. Individuals should avoid sex for at least 2 weeks after the warts have gone away. It is still possible to spread the virus to others after this time, so it is important to use barrier protection when having sex.  3. Syphilis Syphilis is a severe bacterial infection and another type of STI. In the early stages of infection, syphilis usually causes a hard, painless, red sore on the penis. This sore lasts for 3–6 weeks. Untreated, syphilis can lead to: cardiovascular problems dementia hearing or vision loss increased risk of HIV infection meningitis pregnancy, childbirth, and fetal complications stroke Treatment If a person suspects syphilis, they must seek medical attention as early as possible to prevent the infection from progressing and causing severe, lasting health complications. A penicillin injection is the main form of treatment for syphilis.  4. Scabies Scabies is a contagious skin condition that can affect many parts of the body, including the penis. People get scabies when the Sarcoptes scabiei mite burrows into the skin. Sexual contact increases the risk of scabies in the penis. Scabies causes tiny blisters or sores on the skin that are extremely itchy, especially at night. These sores typically occur in thin, irregular lines showing the path of the mite under the skin. After an infestation occurs, a person who has never had scabies before may not develop symptoms until after 4–6 weeks. Symptoms typically show up within 1–4 days in cases of a second or subsequent infestation. Treatment Prescription creams and lotions are the first line of treatment for scabies. If these do not work, a doctor may prescribe oral medications. Cold compresses and antihistamines can relieve itching until the scabicide medication takes effect.  5. Molluscum contagiosum Molluscum contagiosum is a viral skin infection. Anyone can catch molluscum contagiosum from direct contact with others or from sharing towels or personal items. Sexual contact can cause it to develop on the penis. Symptoms include itchy, round, raised, pink or flesh-colored sores on the penis. These can occur alone or in clusters. Many cases clear up without treatment within 12–18 months. While sores are present, people can transmit molluscum contagiosum to others. Treatment To remove the sores and to avoid transmitting the infection to others, doctors recommend: topical creams or lotions surgical removal of the lesions with a curette, which is a small hooked tool cryotherapy laser surgery  6. Chancroid Chancroid is a bacterial infection that the Haemophilus ducreyi bacterium can cause. It spreads from one person to another through sex without barrier protection. The infection causes small, red, raised sores to form on the penis. These are itchy and painful, and they ooze blood or other fluid when they later open and become ulcerative. Other symptoms include pain during sexual activity or urination, and swelling in the groin. Treatment As with other bacterial infections, the main treatment for chancroid is antibiotic medication. Treatment can cure the infection and prevent it from spreading to others. Chancroid is a risk factor for HIV infection.  7. Granuloma inguinale Granuloma inguinale is a bacterial STI that causes ulcers to form on the genitals and anus. It is rare in the U.S., but common in some developing regions. In the beginning, the infection causes small, painless bumps. Over time, these sores slowly develop into deepening ulcers that bleed. Treatment Antibiotics treat the infection and reduce the risk of scarring. 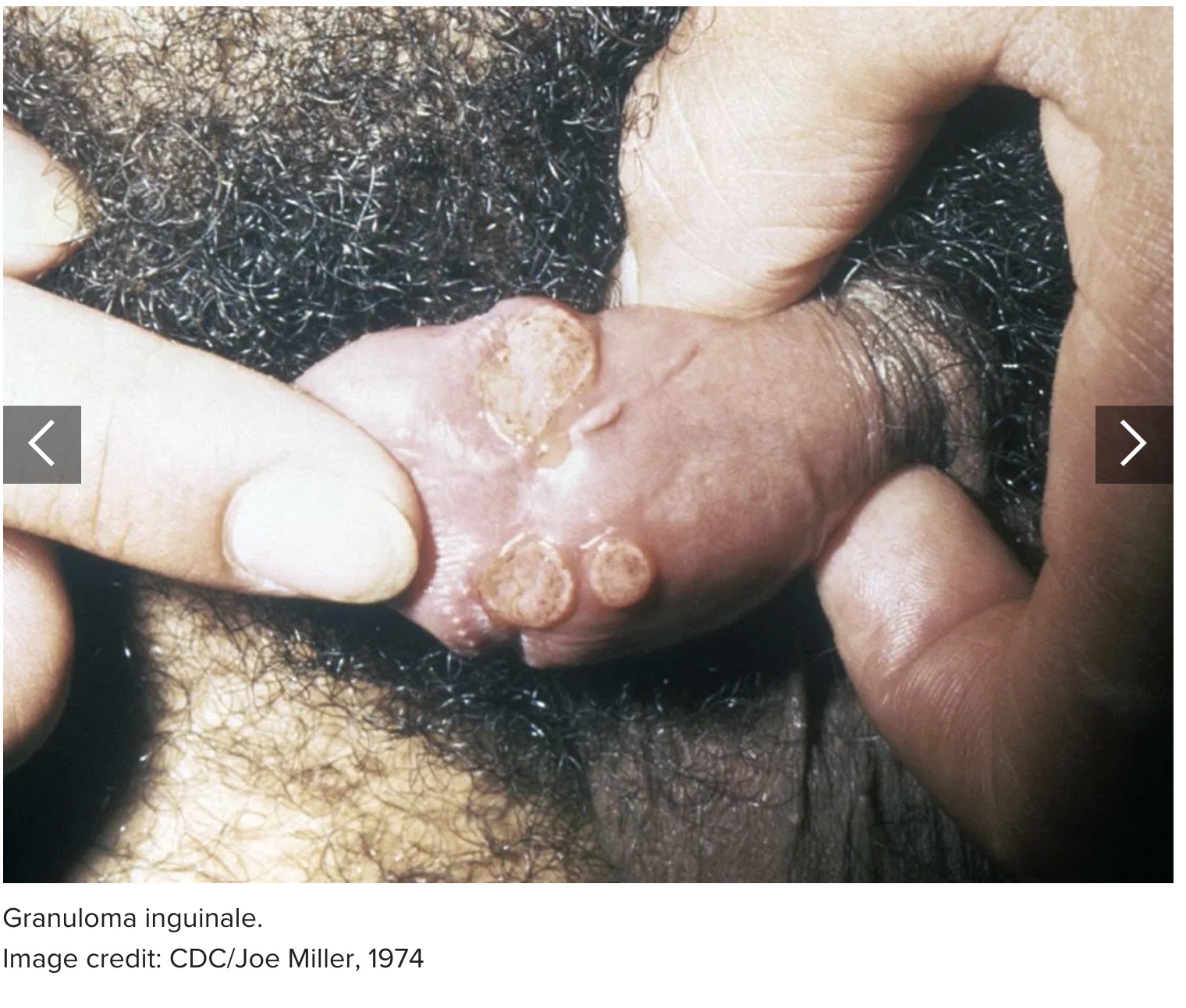 8. Psoriasis Psoriasis is an autoimmune skin condition that causes red, scaly patches of skin. On the penis and genitals, it can cause: a red rash with silvery scales dry, cracking skin that may bleed itching, pain, and discomfort Symptoms vary from one person to another. In some, it may appear as just a few spots, while others experience a widespread rash. Treatment There is no cure for psoriasis, but treatment aims to keep symptoms under control. Medical treatments include: topical creams and ointments oral medications injected medications UV light therapy Lifestyle changes and home remedies can relieve discomfort. These include cool compresses, moisturizing lotions, and stress management. 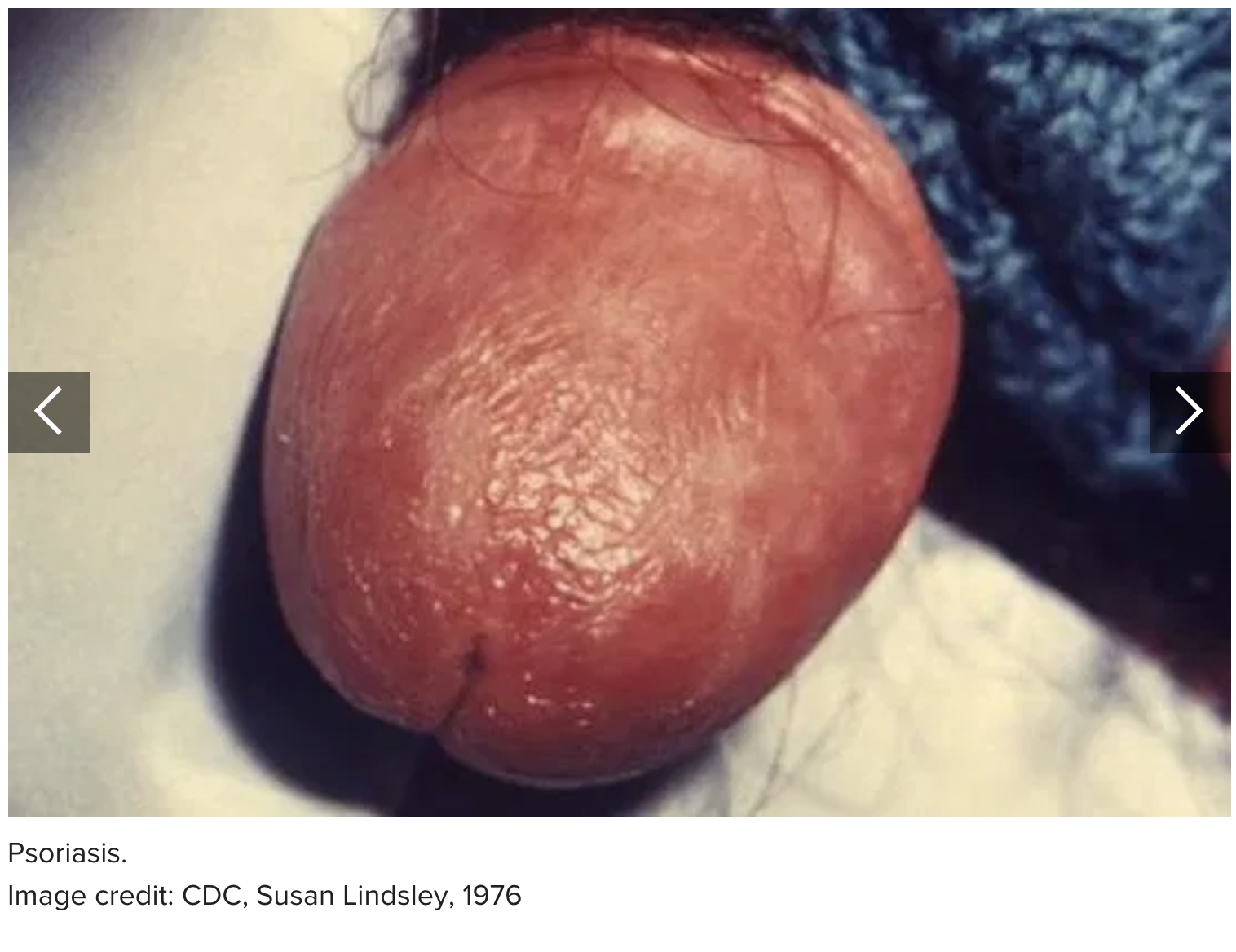 9. Atopic dermatitis Atopic dermatitis, or eczema, is a chronic skin condition. It can affect many body parts, including the penis. An eczema rash causes red, flaky bumps that itch. The bumps may blister and burst before forming a scab. Eczema occurs in people who have a gene variant that affects their skin's ability to protect against irritants and allergens. Eczema rashes on the penis may result from contact with scented cleansing products, laundry detergents, or from chafing from clothing. Treatment Mild eczema may respond to the following home remedies: cool compresses warm oatmeal baths loose clothing moisturizing with an unscented lotion If these do not work, a doctor may prescribe oral or injectable medications or topical creams. Learn more about home remedies for eczema here.  10. Lichen planus Lichen planus is another autoimmune skin condition. It causes an itchy rash characterized by flat, purple-red bumps. The rash may develop on the penis, inner arms, wrists, ankles, or other body parts. These sores may form blisters that ooze and crust over. Painful, white sores that look like lace may also develop in the mouth. Treatment Treatment for mild cases of lichen planus includes oatmeal baths, cool compresses, and over-the-counter (OTC) hydrocortisone creams. If these options do not work, a doctor may prescribe medication. 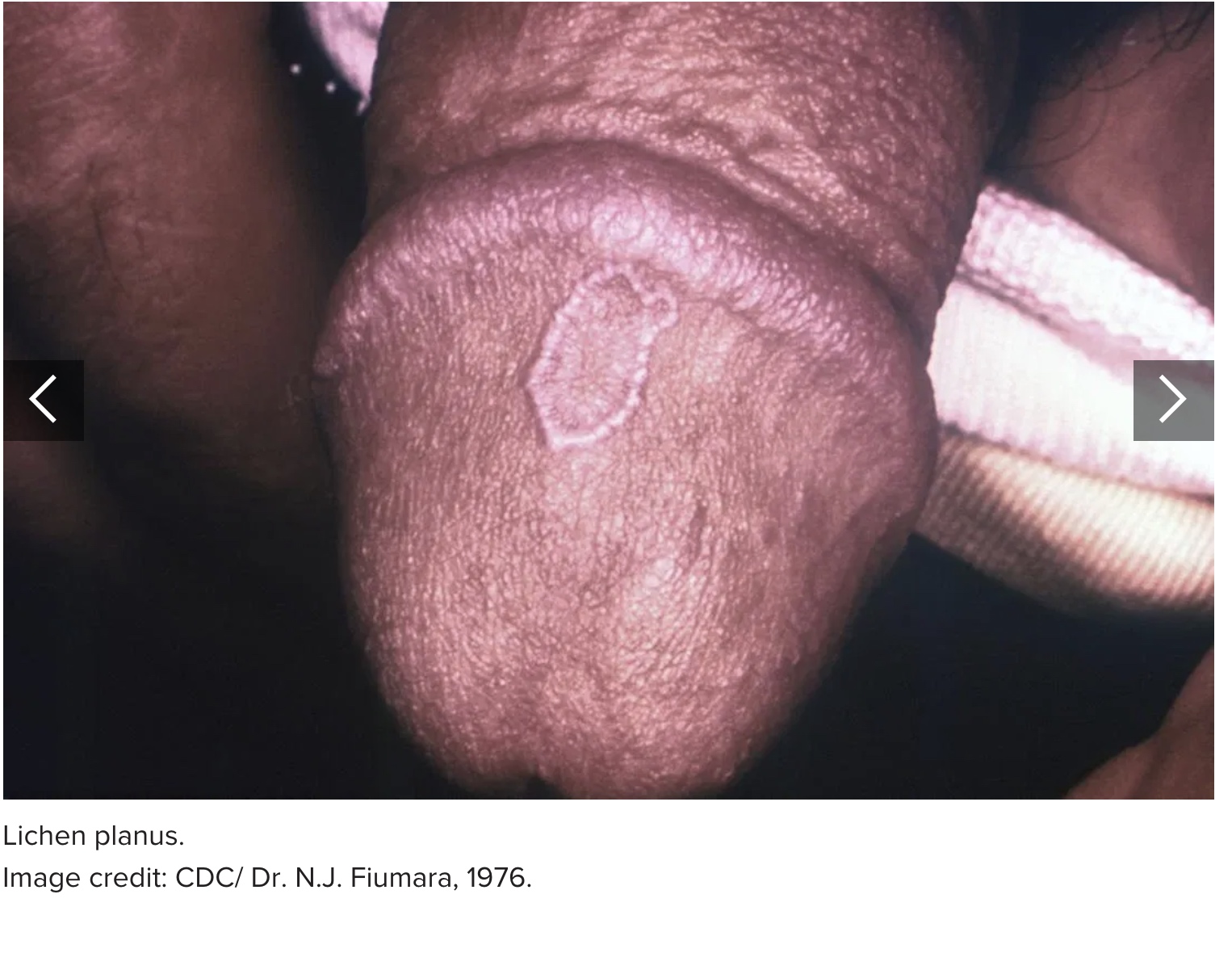 11. Diabetes ulcers Diabetes ulcers typically appear on the feet. However, at least one case report describes penile ulcers as a result of diabetes. In this case, treatment involved antifungal cream and medication to control blood sugar levels. More common symptoms of diabetes mellitus include: slow healing sores on the skin frequent skin infections increased thirst and urination extreme hunger fatigue and irritability blurred vision Treatment Diabetes treatment varies from one person to another. Options include medication, a balanced diet, physical activity, and other lifestyle changes. 12. Penile cancer Penile cancer is a rare form of cancer. Typically, the first symptom is a change in the skin of the penis, such as: a lump or small, crusty sore or ulcer that may bleed changes in skin color thickening of the skin a rash under the foreskin odorous discharge or bleeding under the foreskin flat growths Treatment Penile cancer requires prompt treatment to stop it from progressing. A doctor may recommend one of the following options: surgical removal of the foreskin or cancerous tissue chemotherapy radiation therapy  Outlook The outlook for people with penis sores depends on the underlying cause. Typically, penis sores occur due to a STI or chronic skin condition. It is important to avoid sexual activity until a doctor determines the precise cause of the sores. Seek prompt medical attention if other symptoms accompany the sore, such as: painful urination or ejaculation unusual discharge from the penis or the sores fever or chills fatigue or a general feeling of illness unexplained weight loss The earlier a person seeks treatment, the better the outcome.
__________________
You are my forum, my only forum, you make me happy, when skies are grey... Sex health related questions click here. WOMEN'S CHARTER click here Sg law on sex related matters click here Last edited by Big Sexy; 22-01-2020 at 12:50 PM. |
|
#247
|
||||
|
||||
|
Re: Sexual Health News
How often should a man release sperm?
https://www.medicalnewstoday.com/articles/326586.php Medically reviewed by Kevin Martinez, M.D. on October 8, 2019 Written by Zawn Villines For most men, ejaculating is synonymous with having an orgasm, although some men can have an orgasm without ejaculating. Ejaculate contains fluid from the prostate, seminal vesicles, and bulbourethral glands. Though it contains a wide variety of substances, including citric acid, cholesterol, mucus, and water, its primary job is to deliver sperm. Research shows that the frequency with which a man ejaculates may affect his health, sperm count, and overall well-being. While no evidence says that not ejaculating causes serious health problems, frequent ejaculation may reduce a man's risk of prostate cancer. Having satisfying sex with a partner may also improve a man's health. This article looks at how often a man should release sperm, whether there is a link between ejaculation and cancer, and the effects of ejaculation on the body. What is normal? Many men may wonder whether their sexual behavior is normal. They may fear that they are not having as much sex as their peers, or that they are masturbating too frequently. The truth is that there is no "normal" number of times a man should ejaculate. Average ejaculation frequency varies according to many factors, including a man's: age health relationship status According to the 2015 Sexual Exploration in America Study, partnered sex and the ejaculation that usually accompanies it is most frequent among men ages 2529, with 68.9% reporting vaginal intercourse during the last month. The figure drops slightly to 63.2%, among men in their 30s, and declines with each decade of advancing age. Research published in the Journal of Sexual Medicine found that masturbation was common across a man's lifespan. Men of all age groups reported masturbation in the past month. Solo masturbation was more common than partnered sex during adolescence and in those about 70. Partnered masturbation was highest among men ages 3039. What is safe? No guidelines state the ideal frequency with which a man should ejaculate, whether on his own or with a partner. Myths exist about the dangers of regular masturbation. However, according to Planned Parenthood, there is no evidence that frequent masturbation is harmful. Likewise, most people do not consider frequent consensual sex with a partner to be harmful to either party as long as both partners: feel comfortable in their actions avoid sexual activities that cause pain adopt safer sex strategies A 2015 study found that men who ejaculated daily over 14 days experienced slight decreases in the number of sperm in their ejaculate. However, the reduction did not cause sperm count to fall below normal thresholds. Also, frequent ejaculation did not affect other measures of sperm health, such as sperm motility and morphology. Research published in the journal Social Psychological and Personality Science found that partners who have sex at least weekly report being happier with their relationships. More frequent sex did not increase relationship satisfaction, but it also did not cause it to decline. Is there a cancer link? Men who ejaculate frequently may have a lower risk of prostate cancer, according to a 2016 study that followed men for nearly 2 decades. Researchers found that men ages 4049 that ejaculated more frequently had a lower risk of prostate cancer. Men with the lowest risk ejaculated at least 21 times per month. The study did not establish that ejaculation could prevent cancer in younger men. The researchers remain unsure whether frequent ejaculation fights prostate or any other cancer in men under 40. There is no evidence that frequent ejaculation is harmful to younger men. Effects on the body Ejaculation may offer numerous health benefits. Ejaculation from partnered sex may be particularly beneficial because: Sex is a form of exercise. Exercise reduces the risk of cardiovascular disease, obesity, diabetes, and many other health problems. Sex may reduce the risk of cardiovascular disease. Research that followed men with erectile dysfunction found that those who had sex less than once a month were more likely to develop heart disease. Sex may relieve stress and improve mood. Having sex at least once per week may improve the immune system. Ejaculation may offer pain relief for chronic pain and the pain associated with several conditions. Many men also find that ejaculation, whether alone or with a partner, helps them sleep. Men who worry about sperm production should know that the body continually produces sperm. Frequent ejaculation will not cause the body to run out. Although it takes the average sperm about 74 days to fully mature, the body makes millions of sperm each day. Men with healthy, normal sperm counts should not worry about the effects of regular ejaculation. Those with a low or marginal sperm count should discuss ejaculation frequency with a knowledgeable doctor or reproductive endocrinologist. Summary Most research suggests that frequent ejaculation offers several health benefits. There is no evidence that regular ejaculation causes any health issues. More frequent ejaculation may mean a man gains more health benefits. The positive benefits of ejaculation do not mean that all men must ejaculate frequently. Men who prefer to avoid sex, asexual men, men for whom ejaculation is painful, and many other men may find that the discomfort of ejaculation outweighs any benefits. Men who only want to have sex with a partner may limit their ejaculation because of relationship problems, fatigue, or because their partner does not want to have sex. Ultimately, there is no right number of times a man should ejaculate. While frequent ejaculation may offer several health benefits, no evidence proves that never or infrequently ejaculating causes specific health issues. |
|
#248
|
||||
|
||||
|
Re: Sexual Health News
What causes cysts on the penis?
https://www.medicalnewstoday.com/articles/326622.php Medically reviewed by Kevin Martinez, M.D. on October 10, 2019 Written by Jamie Eske Cysts are sac-like structures in the skin that contain fluid, pus, or gas. They usually appear on the face, ears, neck, or back, but they can develop in other areas, including the penis. Most penile cysts do not require treatment. However, anyone who thinks that they may have a cyst should see a doctor for a diagnosis. Sexually transmitted infections (STIs) and other health issues can cause bumps that resemble cysts to form on the penis. The causes of penile cysts vary, and each has distinct symptoms. In this article, we discuss the causes, symptoms, treatment options, and risk factors of penile cysts. Pearly penile papules Pearly penile papules are noncancerous, dome-shaped lesions that develop along the corona, which is the border of the tip of the penis. On average, 1448% of males develop these penile papules, according to one 2016 review of studies published in the American Journal of Men's Health. Pearly penile papules have no known cause. They do not develop as the result of an infection or any other underlying medical issue. Usually, these papules clear up on their own and do not require treatment.  Epidermoid cyst Epidermoid cysts are sac-like structures that contain keratin, which is a fibrous protein. Keratin exists in the hair, skin, and nails. In one 2019 article, researchers report that, while epidermoid cysts can occur anywhere on the body, they usually develop on the: face scalp neck back scrotum These cysts are not typically a cause for concern, but they can become inflamed, which may result in discomfort or pain in the area. 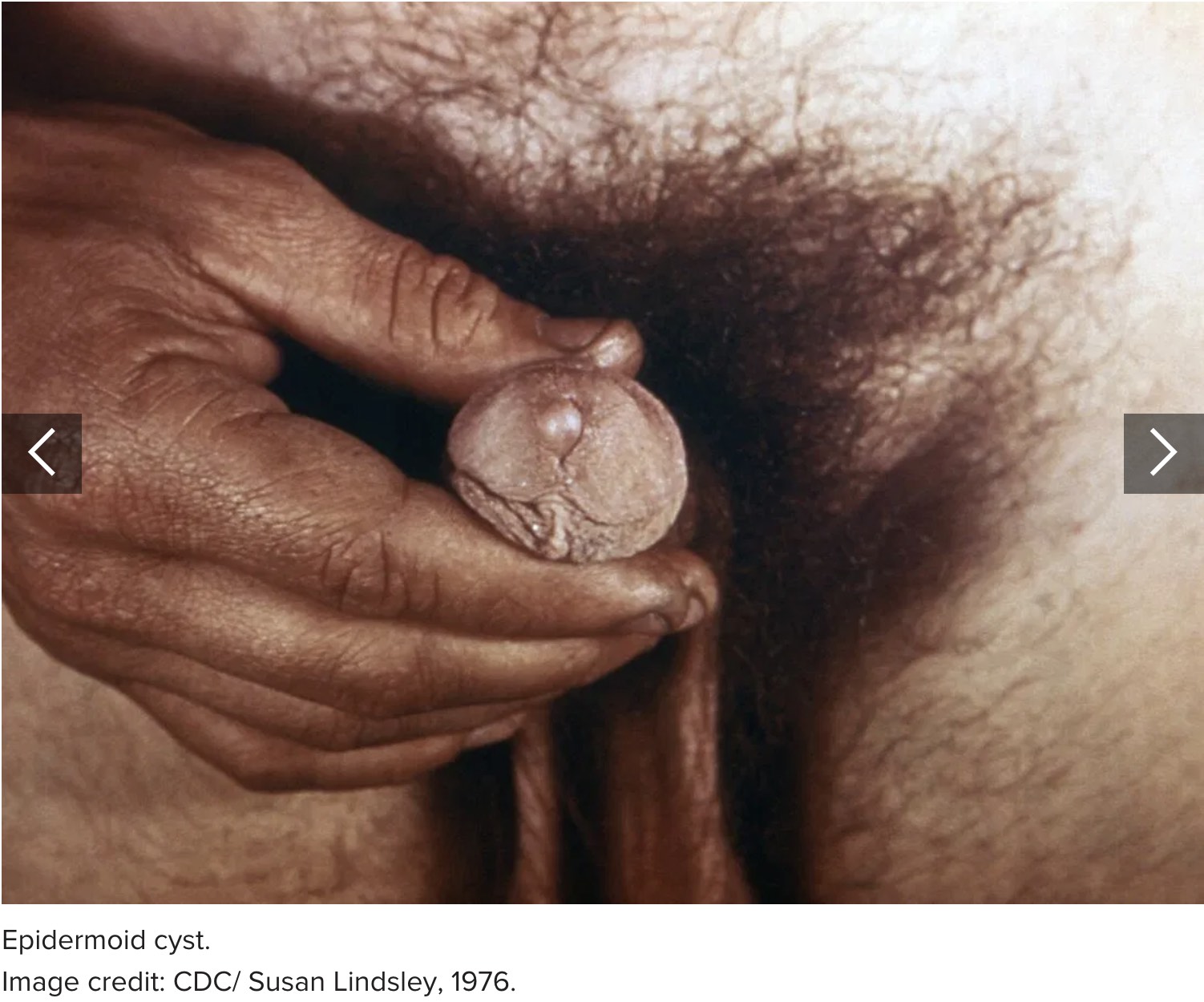 Tyson glands Tyson glands are small, sebaceous glands on either side of the frenulum. The frenulum is the elastic band of connective tissue that connects the foreskin to the penis. If a person has enlarged Tyson glands, they may develop tiny yellow or white bumps on the underside of the penis.  Median raphe cyst Median raphe cysts are rare, and they develop on the bottom of the head of the penis. These cysts form before birth. However, the authors of one 2019 case report note that people tend only to realize that they have median raphe cysts in adolescence or adulthood, or when the cyst grows large enough to cause inflammation in the surrounding skin tissue. Fordyce spots Fordyce spots are small, yellow or white bumps that can form on the lips, inner cheeks, penis, or scrotum. These bumps develop in sebaceous glands that do not contain hair follicles. According to a 2015 case report, Fordyce spots affect 7080% of adults and occur twice as often in males as in females. Fordyce spots may appear during puberty, when fluctuations in hormone levels lead to enlarged sebaceous glands. These spots do not usually require treatment because they do not result from an infection or any other health issue. In rare cases, Fordyce spots on the genitals can cause discomfort or pain during sex.  Penile cancer A lump on the penis can result from penile cancer, which is rare. According to the American Cancer Society, cancers affecting the penis account for fewer than 1% of all cancer diagnoses in males in the United States. Symptoms of penile cancer include: a lump on the penis that may grow larger over time an ulcer or open sore on the penis a rash under the foreskin thickening of the skin on the penis brown, crusty bumps on the penis bleeding or unusual discharge  The American Cancer Society recommend that anyone with a growth or any other abnormality on the penis consult a doctor. They suggest seeing a doctor if any change to the penis lasts longer than 4 weeks. Treatment and removal Usually, cysts clear up on their own without treatment. The following tips can help manage any pain or discomfort while a cyst heals: Keep the skin clean: Gently cleanse the skin around the cyst with warm water and fragrance free, antibacterial soap. Pat the skin dry immediately after washing it. Apply a warm compress: Soak a clean towel or cloth in warm water and wring it out. Place the cloth over the cyst for a few minutes. As the cloth cools, soak it again and repeat. Applying this heat will help drain the cyst. Avoid popping or squeezing the cyst: Squeezing a cyst can cause irritation, which may make it grow larger. Popping a cyst can lead to an infection. Some people ask doctors to remove cysts for aesthetic reasons. The doctor may drain the cyst or surgically remove it. A doctor may recommend draining a cyst if it bursts under the skin or an infection develops. After draining the cyst, a doctor will likely prescribe a course of antibiotics to treat an existing infection and prevent future infections. A doctor can remove a cyst by making a small cut on the skin above the cyst. They will use forceps and a scalpel to remove the cyst and the surrounding tissue. After removing the cyst, they will close the wound with dissolvable stitches. If a person may have an STI, they should see a doctor for an evaluation. Certain STIs can cause cysts to form on the penis. Risk factors The following factors can increase a person's risk of developing a penile cyst: hormonal changes injury to the penis poor personal hygiene vigorous sexual activity genetics or family history Summary Cysts can develop anywhere on the body, including the shaft and head of the penis. Usually, a cyst on the penis does not require medical treatment. People can treat a cyst at home by: keeping the skin around the cyst clean and dry applying a warm compress to help drain fluid from the cyst refraining from popping or squeezing the cyst A person can have a cyst drained or surgically removed if it causes discomfort. |
|
#249
|
||||
|
||||
|
Re: Sexual Health News
Everything you need to know about man boobs
https://www.medicalnewstoday.com/articles/326637.php Medically reviewed by Daniel Bubnis, M.S., NASM-CPT, NASE Level II-CSS on October 11, 2019 — Written by Jenna Fletcher Everyone, including males, has some breast tissue. For many males, the breast tissue never enlarges. For some, however, it expands due to hormonal changes, certain medications, or an underlying medical condition. Some people call this condition "man boobs," which may feel like an uncomfortable or bothersome term. Some males may also feel embarrassed to seek a doctor's advice about enlarged breast tissue. However, it is important to note that enlarged breast tissue is a common concern. As such, there are many possible treatments available for those who wish to change the look of their chest. Keep reading for more information about the causes of male breast expansion and possible exercises, dietary changes, and treatments to reduce their appearance. Causes Testosterone in the male body usually prevents the breast tissue from expanding. However, some males develop enlarged breasts due to hormonal changes or fluctuations. When this occurs, doctors call it gynecomastia. Gynecomastia is more common in certain groups, including: infants, due to their mother's estrogen teenagers, due to changing hormone levels those over the age of 50 There are several potential causes of gynecomastia, including: hormone changes taking certain antibiotics taking medications that block the action of testosterone excessive alcohol consumption taking certain psychiatric medications taking anti-ulcer medications taking herbal supplements that contain phytoestrogens using tea tree oil or lavender lotions using illicit drugs, such as anabolic steroids or androgens excessive body fat liver or kidney disease certain types of tumor overactive thyroid other conditions that cause lower testosterone levels However, for many males, excess breast tissue is not the cause of "man boobs." Like the abdomen, the chest can accumulate fat. In these cases, exercise and dietary changes can reduce their appearance. Exercises When excess fat stores are the cause of male breast expansion, one of the best remedies is a combination of diet and exercise. When exercising, people can focus on both cardiovascular workouts to reduce weight overall and chest exercises that focus on developing the pectoral and other chest muscles. Before starting a new exercise routine, it is best to speak to a doctor to determine what is safe and appropriate for a person's individual needs and abilities. Some cardiovascular workouts and activities for weight loss include: walking running team sports high intensity interval training jogging cycling swimming According to the United States Department of Health & Human Services, an adult should perform 150–300 minutes of moderate intensity exercise or 75–150 minutes of high intensity exercise per week. Although it is impossible for a person to lose weight in a specific place on the body, targeted chest exercises can help them gain more muscle in the chest, which may help reduce the appearance of breast tissue. In addition, the more muscle a person has, the faster their metabolism works and the more calories they will burn. Chest exercises to build muscle include: If a person has a gym membership, they can take advantage of a number of different machines that target the chest muscles. It is always best to talk to a trainer about how to use each machine for maximum benefit and to reduce the risk of injury. Dietary changes If excess weight is causing or contributing to enlarged male breasts, a person can focus on changing their eating habits. In general, the best dietary changes to make are ones that are small and sustainable. Significantly overhauling the diet is often very difficult to maintain and can lead to regaining lost weight. The Centers for Disease Control and Prevention (CDC) recommend losing weight at a rate of around 1–2 pounds per week. Gradual weight loss is more sustainable and can lead to overall health improvements. Before making changes to the diet, it can be helpful to keep a food journal. A food journal can give a person insight into what they can cut out and what nutrients are lacking. The CDC also put together some recommendations for reducing caloric intake. These include: eating whole, raw fruits and vegetables whenever possible avoiding fruit juices, as they do not contain fiber using no or low fat cooking techniques, such as steaming, boiling, or baking choosing whole fruit over dried fruit substituting unhealthful snacks with fruits or vegetables Treatment Treatment options vary based on what is causing the enlarged appearance of male breasts. If it is a matter of extra weight, a doctor may recommend that a person makes changes to their diet and exercise routines. If medications are responsible, a doctor may be able to prescribe alternatives. Sometimes, however, the benefits of a current medication outweigh the side effects. If a medical issue is causing the breast tissue to enlarge, treating the underlying condition can help. Some people may choose to undergo surgery to remove the excess breast tissue. However, unless it is for the treatment of breast cancer, insurance companies tend to consider the removal of male breast tissue a cosmetic issue and will not cover the costs. Summary All males have some breast tissue. However, some medical conditions, medications, and hormonal changes can cause male breasts to grow larger than usual. In other cases, excess weight in the area may make the breast tissue look as though it has grown. People put on weight in different places, and some people first put on weight in their breast area. If enlarged male breasts do not reduce with dietary changes, exercise, or other treatments, a person may consider surgery to reduce the appearance. |
|
#250
|
||||
|
||||
|
Re: Sexual Health News
Most common 3 STDs on the rise, according to CDC report
https://www.medicalnewstoday.com/articles/326604.php#1 Written by Tim Newman on October 11, 2019 - Fact checked by Paula Field According to a report published this week by the Centers for Disease Control and Prevention, the number of people with chlamydia, gonorrhea, and syphilis is rising. Yesterday, the Centers for Disease Control and Prevention (CDC) released its annual Sexually Transmitted Disease Surveillance Report, containing data from 2018. In it, they outline some worrying trends in the numbers of sexually transmitted diseases (STDs). According to the report, the combined number of syphilis, gonorrhea, and chlamydia cases reached an all time high in 2018. In a companion press release, Dr. Gail Bolan, Director of the Division of Sexually Transmitted Disease Prevention, writes that this is the "fifth consecutive year of increases" for the three STDs. STDs in numbers Between 2017 and 2018, the number of gonorrhea cases increased by 5% to a total of 580,000 cases; this is the highest number of cases since 1991. As for chlamydia, cases hit the highest numbers ever recorded by the CDC. Compared with 2017, they were 3% higher, making a total of 1.7 million cases. The number of primary and secondary syphilis cases, which are the most infectious stages of syphilis, increased by 14% to 35,000 cases; this is also the highest level since 1991. Syphilis can pass between a mother and her unborn child, which doctors refer to as congenital syphilis. In 2018, there were 1,300 cases of syphilis in newborns, an increase of 40%. In all, 70% of congenital syphilis cases occurred in five states: California, Florida, Texas, Arizona, and Louisiana. Congenital syphilis increases the risk of stillbirth, miscarriage, newborn death, and lifelong medical issues. There was an increase in newborn deaths from 77 in 2017 to 94 in 2018. Dr. Bolan injects the statistics with emotion: Quote:
These increases are particularly striking given that STDs had, seemingly, been on the ropes. As the CDC report states in the foreword written by Dr. Bolan, "not that long ago, gonorrhea rates were at historic lows, and syphilis was close to elimination." Why the increase? Several factors are likely to play a part in the increase in STDs. According to the CDC press release, these factors include poverty, drug use, and unstable housing, all of which "reduce access to STD prevention and care." The CDC also noted a reduction in condom use among some at risk demographics, such as young people, and gay and bisexual men. Added to this, the CDC explain in the press release how certain financial restraints have played a part: Quote:
According to the CDC report, reversing these changes will take pointed, combined efforts from multiple stakeholders. They call for "federal, state, and local programs [to] employ strategies that maximize long term population impact by reducing STD incidence and promoting sexual, reproductive, maternal, and infant health." They explain that as health infrastructure erodes, fragile populations are missing out on the healthcare and preventive services that they deserve. The CDC also explain the need for increased surveillance. It is imperative that reports do not only count those who have access to treatment and diagnosis. It is crucial to uncover hidden populations; otherwise, it is impossible to prevent infections from spreading. According to the CDC, healthcare providers should make STD screening and treatment a "standard part of medical care." They also place pressure on state and local health departments, asking them to "strengthen the local public health infrastructure" to stem the tide of STDs and protect the most vulnerable members of society. The take-home message of the report is that it is crucial to take action. However, Dr. Bolan ends her press release with positivity: "Together, we can turn the tide to protect the people we diligently serve day in and day out." |
|
#251
|
||||
|
||||
|
Re: Sexual Health News
Can males get bacterial vaginosis?
https://www.medicalnewstoday.com/articles/326662.php Medically reviewed by Alana Biggers, M.D., MPH on October 14, 2019 Written by Danielle Dresden Bacterial vaginosis (BV) is an infection in the vagina. Males cannot develop bacterial vaginosis, but they can spread the infection. According to the Centers for Disease Control and Prevention (CDC), BV is the most common form of vaginal infection for women between ages 15 to 44. People with BV can get symptoms that include excess and discolored discharge from the vagina. It can cause a burning or itching sensation around the vagina, especially when urinating. Currently, doctors are unclear exactly how the infection starts. But having sex with multiple partners or the regular use of douches that upsets the healthy vaginal flora may be responsible. Sex with both males and females can increase the risk of BV to spread. In this article, we discuss what BV is, how males can transmit it, and treatments. Is bacterial vaginosis in males possible? BV is an infection that occurs in the vagina. But males can carry the bacteria that cause BV. The bacteria can accumulate on the penis or in the urethra of males. This means that people carrying the bacteria can transmit it to females by having sex with them. The closest condition to BV in males is urethritis. This is where the urethra becomes inflamed. The urethra is a tube connecting to the bladder that helps to remove urine from the body. Both males and females have a urethra. Urethritis is a common condition that affects roughly 2.8 million males in the United States each year. Doctors are unclear what causes urethritis in about 45% of these cases. Researchers are now exploring associations between BV and urethritis, where there is no clear cause. Symptoms Bacterial vaginitis does not cause many symptoms, and those that do develop are typically mild. Some people may not notice any symptoms at all. Some symptoms of BV include: more vaginal discharge than usual gray-white or yellow vaginal discharge unpleasant smells coming from the vagina, especially after sexual activity Without treatment, BV can have more severe consequences. For example, a person with BV may have an increased chance of developing HIV if they have sexual intercourse with someone who has HIV. Having BV also increases the chances of getting sexually transmitted diseases (STDs), such as chlamydia. Pregnant women can also get BV. When this happens, women are more likely to give birth early or to a baby with low birth weight. Pregnant women should make sure they get treatment for BV to avoid these complications. Urethritis can occur in males and females. In males, symptoms of urethritis include: discharge from the penis blood in the semen or urine pain or burning while urinating itching around the penis or urethra For females, the symptoms include: excess discharge from the vagina pain or burning during urination regularly needing to urinate irritation around the vagina Anyone with these symptoms should see a doctor for treatment. Causes and treatments The infection that causes BV is the result of an overgrowth of certain bacteria coming into contact with the vagina. Bacteria that leads to BV include: Leptotrichia Sneathia Atopobium Megasphaera Clostridiales Doctors are unclear exactly how these bacteria come into contact with the vagina. People with multiple sexual partners will increase their chances of getting BV. Using douches may also increase the chances of BV. It is possible for douching to upset the balance of bacteria in the vagina, leading to BV. Males whose sexual partners have BV are more likely to have these bacteria on the tip of their penis and in the urethra. Those who are circumcised are less likely to carry these bacteria on their skin. Doctors will treat BV with antibiotics. They may prescribe a pill or antibiotic creams or gels for applying directly to the vagina. These antibiotics help the body kill bacteria causing BV. Antibiotics are effective in treating BV. But it is still possible for the infection to return after treatment. People should talk to their doctor about the use of probiotics to help with BV. Prevention It is often difficult for a person to prevent BV because the exact causes remain unclear. But the following tips can reduce the risk of BV occurring: using condoms during any sexual activity cleaning sex toys after use limiting the number of sexual partners avoiding the use of douches washing the vagina regularly with only warm water wearing underwear made from cotton or with a cotton lining Outlook Sometimes BV will go away on its own. But anyone who experiences symptoms should see a doctor for treatment. In most cases, antibiotics will kill the bacteria quickly, and the symptoms will go away. People who have had BV are more likely to get the infection again. It is essential to treat the condition every time it occurs. This will reduce the risk of complications, such as other STDs. |
|
#252
|
||||
|
||||
|
Re: Sexual Health News
Reasons for discharge in males
https://www.medicalnewstoday.com/articles/327228.php Medically reviewed by Kevin Martinez, M.D. on December 5, 2019 Written by Hannah Nichols Male discharge is any fluid that comes from the urethra other than urine. The urethra is a narrow tube that carries urine from the bladder and semen from the ejaculatory ducts. These fluids travel along the urethra before exiting the body at the urethral opening in the tip of the penis. Some types of discharge are natural and help protect or lubricate the penis. Others may occur as a result of an underlying health condition. These may be accompanied by symptoms such as pain, irritation, or an unpleasant smell. This article describes the types of penile discharge that doctors consider normal and those they consider to be abnormal. We outline the symptoms associated with each and provide information on when to see a doctor. What is normal discharge? Normal discharge includes preejaculate and ejaculate. These are released from the tip of the penis during sexual arousal and intercourse. Although not strictly penile discharge, smegma is another substance that may build up around the head of the penis. The sections below will cover these types of normal male discharge in more detail. Preejaculate Preejaculatory fluid, or precum, is a thick alkaline mucus produced in the bulbourethral glands. The bulbourethral glands, or Cowper's glands, are two pea-sized glands located below the prostate gland. During sexual stimulation, the bulbourethral glands secrete up to 4 milliliters (ml) of preejaculate into the urethra. Preejaculatory fluid may: function as a lubricant for semen lubricate the tip of the penis during intercourse neutralize acidity left by urine residue in the urethra neutralize vaginal acidity Whereas the bulbourethral glands release preejaculatory fluid, it is the testes that release sperm. Nonetheless, a 2011 study found that some preejaculate contains live sperm. Preejaculatory samples from the participants contained up to 23 million sperm. Researchers are not sure whether preejaculate is contaminated immediately before ejaculation or contaminated with sperm leftover from a previous ejaculation. Ejaculate Ejaculate, or semen, is a milky, cloudy fluid that travels through the urethra and out of the penis following sexual stimulation. This process is called ejaculation, and it usually happens during orgasm. Healthy sperm concentrations in semen are around 15150 million sperm per ml of semen. Sperm are produced in the testes. They then mature inside ducts located behind the testes. These ducts are called the epididymis and the vas deferens. During sexual stimulation, the sperm mix with seminal fluid to form semen. Seminal fluid is a whitish liquid produced by the prostate glands and glands called the seminal vesicles. Sperm make up a small part of semen. Semen is composed of the following: 15% sperm around 5% secretions from the bulbourethral glands 1530% secretions from the prostate fluid from the seminal vesicle Smegma Smegma is a thick, white substance made up of skin cells, skin oils, and moisture. It is secreted by the sebaceous glands in the skin around the genitals. In males, smegma tends to build up between the head of the penis and the foreskin. Smegma is a natural lubricant that helps keep the genitals moist and enables the foreskin to retract during sexual intercourse. However, smegma buildup may produce a foul odor and can act as a breeding ground for bacteria. Washing the penis once per day with clean, warm water will help reduce smegma buildup. That said, males should avoid washing the penis too frequently with soap or shower gel, as these products can cause irritation and soreness. What is abnormal discharge? The presence of male discharge at times other than sexual stimulation may signal an underlying health concern. We describe some of these in the sections below. Balanitis Balanitis refers to inflammation of the skin around the head of the penis. When the inflammation also affects the foreskin, it is known as balanoposthitis. Some symptoms of balanitis include: thick, lumpy discharge that is either white or yellow an unpleasant smell a red, inflamed rash or swelling irritation, soreness, itching, or burning pain when urinating Many factors can cause balanitis, including: Poor hygiene: The area underneath the foreskin requires regular cleaning. Dead skin cells, urine residue, and sweat provide the ideal environment for irritation-causing bacteria to breed. Allergies: Urine, soaps, condoms, and lubricants can irritate the skin on the penis. Skin conditions: Eczema, psoriasis, or lichen sclerosus may cause redness and inflammation. Infection: Bacterial or fungal infections can make the head of the penis sore, tender, and itchy. Sexually transmitted infections (STIs): STIs such as herpes simplex virus (HSV) can cause blistering and inflammation in the area around the genitals. Both circumcised and uncircumcised males can develop balanitis. However, one 2017 study found that balanitis is 68% less prevalent among circumcised males than uncircumcised males. Trichomoniasis Trichomoniasis is a common infection that affects around 3.7 million people in the United States. The parasite Trichomonas vaginalis causes trichomoniasis. Around 70% of people with trichomoniasis do not experience any symptoms. If symptoms do occur in males, they may include: thin, white penile discharge a frequent need to urinate a burning sensation when urinating pain during ejaculation swelling around the head of the penis or the foreskin Urethritis Urethritis is characterized by inflammation of the urethra, and it can be infectious or noninfectious. Urethritis often develops as a result of an STI. If it develops due to gonorrhea, it is called gonococcal urethritis. If the cause is unknown, it is called nongonococcal urethritis. Over 40% of people with nongonococcal urethritis do not experience symptoms. However, some males may experience the following symptoms: cloudy or white discharge from the tip of the penis irritation and soreness at the urethral opening a burning sensation when urinating a frequent need to urinate testicular pain or swelling The following pathogens can also cause urethritis: Neisseria gonorrhoeae Chlamydia trachomatis Mycoplasma genitalium Trichomonas vaginalis HSV Epstein-Barr virus adenovirus C. trachomatis is the most common cause of nongonococcal urethritis. It accounts for around 1540% of cases. Urethritis can also result from vigorous sex, masturbation, and urinary tract infections (UTIs). UTIs UTIs are a common type of bacterial infection. They affect part of the urinary system. The urinary system includes the bladder, kidneys, and urethra. UTIs occur when bacteria from the skin or rectum enter the urethra and cause infection in the urinary tract. UTIs tend to be more common in females, who have shorter urethras that are closer to the rectum. This makes it easier for bacteria to enter the urethra and reach the bladder and kidneys. However, males can also develop UTIs. Males with a UTI may experience symptoms such as: cloudy urine that contains pus red, pink, or brown urine that contains blood pain or a burning sensation when urinating a need to urinate more than usual strong-smelling urine nausea or vomiting Factors that increase the risk of developing a UTI include: engaging in unprotected sexual activity, particularly with a new partner having had a previous UTI having kidney stones having an enlarged prostate having a weakened immune system from diabetes, HIV, or chemotherapy using a urinary catheter A person cannot pass a UTI to a sexual partner. However, the person may experience pain and discomfort during sex. STIs STIs can spread from person to person as a result of unprotected sexual activity and genital contact. STIs that may cause abnormal penile discharge include: Chlamydia Chlamydia is the most reported STI in the U.S. However, most people with chlamydia are unaware that they have it, as it often does not cause any symptoms. C. trachomatis is the cause of chlamydia. These bacteria can infect the urethra, rectum, and throat. In males, chlamydia may cause the following symptoms: white, cloudy, or watery penile discharge itching or burning at the tip of the penis a burning sensation when urinating testicular pain Gonorrhea Gonorrhea is a common infection in the U.S., particularly among adolescents and young adults. N. gonorrhoeae is the cause of gonorrhea. These bacteria can infect the urethra and rectum. Sometimes, the infection may also affect the eyes, throat, and joints. Symptoms of gonorrhea in males include: white, yellow, or green penile discharge inflammation of the foreskin pain or a burning sensation when urinating swelling in one testicle When to see a doctor A male should see a doctor if they experience discharge from the penis that is not any of the following: urine preejaculate ejaculate smegma To determine what is causing the penile discharge, a doctor may: ask about the person's symptoms make a note of their medical and sexual history examine the affected area of the penis ask for a urine sample to identify signs of a UTI swab the affected area and analyze the swab for bacteria and viruses After identifying the cause of the discharge, the doctor will determine the best course of treatment. Summary Discharge from the penis that happens during sexual arousal, as a result of sexual intercourse, and after ejaculation is normal. Abnormal discharge tends to: have an unusual color have a foul odor occur without sexual activity be accompanied by pain, burning, or other symptoms In these instances, the discharge could be a sign of a medical condition that needs evaluation and treatment. It is important to make an appointment with a doctor. |
|
#253
|
||||
|
||||
|
Re: Sexual Health News
What are the stages of puberty?
https://www.medicalnewstoday.com/articles/327299.php Medically reviewed by Karen Gill, M.D. on December 12, 2019 — Written by Beth Sissons Everyone goes through puberty slightly differently, but there are puberty stages that usually happen at certain ages in a young person's development. In this article, we look at the stages of puberty for males and females, and the ways that parents and caregivers can help to support kids through this time. Females, stage by stage People's experience of puberty varies. Females start puberty sooner than males. Puberty in females most often begins between the ages of 8 and 13 years. The process may continue until they are 14 years old, although this can be later. The first stage of puberty includes prepuberty changes. These are changes that start to happen in the body but are not yet visible. One of the first physical changes females will notice during puberty is their breasts starting to grow. The initial stage of growth is breast buds. Slight swelling appears under the nipple, and the area of skin around the nipple, known as the areola, will start to get bigger. The breasts will then slowly start to grow during puberty. Females may experience some tenderness or itchiness as the breasts begin to change. It is usual for each breast to grow at slightly different rates, which will often even out over time. Females will also start to notice more hair growing in places such as their legs and arms. At around 12 years old, on average, females will begin to see hair growth under the arms. Pubic hair will start growing along the labia and will gradually become thicker, curlier, and cover a larger area of the vulva. In the final stages of puberty, pubic hair may grow around the top of the thighs. Females will usually begin their period roughly 2 years after their breasts have started to grow. They might get their first period anywhere between 10 and 16.5 years old. It is also normal for females to have white vaginal discharge. Females will also grow taller in puberty, with a gradual height increase each year. In the first stages of puberty, females may grow 5–6 centimeters (cm) in a year. In the following stages of puberty, this can increase to 7–8 cm per year. Females will usually stop growing around 16 years of age. Females may also increase in weight and have more body fat around the upper arms, thighs, and back. Hips tend to become wider, while the waist narrows. At 17–18 years old, breasts are usually fully developed. Breasts can continue to grow up until the early 20s, though. Males, stage by stage One of the first changes in males during puberty is the scrotum enlarging and becoming darker. Once the scrotum and testes begin growing, the penis also starts to grow. Males will start growing pubic hair at the base of the penis, which will then gradually cover a larger area around the genitals. As pubic hair grows, it becomes darker and coarser. In the later stages of puberty, pubic hair may spread to the thighs and stomach. Males will also have hair growth under their arms, legs, and usually on their face and chest. In the first stages of puberty, males may grow in height by about 5–6 cm. In later stages of puberty, this can increase to 7–8 cm and then 10 cm per year. Males will usually stop growing around 17 years old. Height changes can happen in growth spurts, where teenagers may grow very quickly over several months. A period of slower growth may then follow. Males also become more muscular during puberty. Hormonal changes during puberty can sometimes cause slight breast swelling in males. Breast swelling is a common and temporary stage of male puberty. As the voice begins to deepen, males may find their voice "breaks." This means the voice may go through a period of switching between sounding deep and high before it becomes permanently deeper. Males may start having erections as the body begins to produce sperm. Males may also have ejaculations while they sleep, which people may refer to as "wet dreams." Possible complications Some people may experience puberty later or earlier than usual. This can sometimes be a sign of an underlying medical condition, so people should see their doctor. If people experience puberty early, a doctor may refer to this as precocious puberty. In females, early puberty is the appearance of puberty signs and symptoms before the age of 8, such as: ovulation and menstruation underarm and pubic hair breast development For males, early puberty is the appearance of puberty signs and symptoms before the age of 9, such as: a deepening voice pubic and underarm hair enlarged testicles and penis facial hair acne sperm production Early puberty may be a result of an underlying medical condition. Some causes of early puberty include: an issue with the central nervous system genetic syndrome a family history of the condition tumors or growths affecting either the ovaries, brain, pituitary gland, or adrenal glands early release of puberty hormones with no known cause Delayed puberty means there are no physical signs of puberty in females by the age of 13 or males by 14 years old. Symptoms of delayed puberty in females include: more than 4 years between the first signs of breast growth and their first period no breast development by age 13 years no menstruation by 14 to 16 years old Symptoms of delayed puberty in males include: no testicle enlargement by 14 years of age longer than 4 years to reach the adult genital development stage no pubic hair by age 15 years If people have signs of delayed puberty, they may want to see their doctor. Causes of delayed puberty can include: a family history of delayed puberty chromosomal or genetic disorders chronic illness tumors affecting the pituitary gland or hypothalamus, a part of the brain that affects hormones Parental advice Kids go through many physical and emotional changes during puberty and may experience: mood swings depression anxiety low self-esteem self-consciousness aggression body image issues Both males and females may develop acne during puberty. This is because of their body changes and increases in hormone production. These developments can create excess oil, which contributes to the start of acne. Washing the face daily with a cleanser may help to keep acne under control. During puberty, people also start to sweat more. Daily hygiene is essential and may help prevent body odor. Young people may want to start using deodorant. Sometimes, certain body parts, such as hands, feet, arms, and legs, will grow more quickly than the rest of the body. This may cause temporary clumsiness and a slight lack of coordination. Parents and caregivers may want to discuss these issues with their teenagers to ease any embarrassment or anxiety they may feel about their changing bodies. Teenagers may start experiencing romantic or sexual feelings for people of the opposite or same sex. Some teenagers may also feel uncomfortable about their assigned gender. Talking through these issues with teenagers and giving them plenty of support can help them address any anxiety or confusing emotions they may be experiencing through puberty. Advice from Planned Parenthood, which discusses how to talk through puberty with teenagers, may be helpful. Summary Although everyone will experience puberty slightly differently, particular physical changes occur that signal puberty. If people experience puberty symptoms a lot later or earlier than the standard stages, it may indicate an underlying medical condition, and people should see their doctor. Some individuals may feel anxious or embarrassed about the changes to their bodies during puberty. Parents and caregivers may find that discussing the stages of puberty with their preteen or teenager might help to ease their worries. |
|
#254
|
||||
|
||||
|
Re: Sexual Health News
What to know about peeing after sex
https://www.medicalnewstoday.com/articles/327380.php Medically reviewed by Debra Sullivan, Ph.D., MSN, R.N., CNE, COI on December 23, 2019 Written by Beth Sissons People may have heard that peeing after sex is beneficial, especially for women. This is because peeing flushes bacteria out of the body, which may help prevent a urinary tract from developing. Here, we look at how peeing after sex may help to prevent urinary tract infections. We also discuss whether there are any other benefits to peeing after sex. Benefits of peeing after sex Peeing after sex may reduce the risk of developing a UTI. Sexual intercourse is a risk factor for urinary tract infections (UTIs). During sex, bacteria can pass from the genitals to the urethra. The urethra is the tube that connects the bladder to the urethral opening where urine comes out. Bacteria can then make its way from the urethra to the bladder, resulting in a UTI. Peeing after sex helps to flush bacteria out of the urethra, helping to prevent UTIs. How can it help prevent UTIs? Females are up to 30 times more likely to get a UTI than males. This is due to two reasons: Firstly, the female urethra is close to the vagina and anus. This means that bacteria can easily spread from these areas to the urethra. Secondly, the urethra is shorter in females than it is in males. This means that bacteria that enter the urethra can reach the bladder more easily. In women, peeing after sex can help to flush any bacteria away from the urethra. For males, peeing after sex is less important. This is because males have a longer urethra. As a result, bacteria from the genital area is less likely to reach the bladder. Although there is no solid evidence to confirm that peeing after sex can prevent UTIs, there is no harm in following this practice. It may help to reduce the risk of UTIs, especially in women and people who are more prone to UTIs. Does it prevent pregnancy? Peeing after sex will not prevent pregnancy. The urethra and vagina are separate parts of the female anatomy. As a result, peeing will not affect any sperm that enter the vagina. Using some form of birth control is the only way to prevent pregnancy during sex. Does it prevent STIs? Peeing after sex does not prevent sexually transmitted infections (STIs). People contract STIs by absorbing bacteria through the mucous membranes inside their bodies during sexual intercourse. Peeing after sex will not prevent these bacteria from entering the body. Using a condom or other form of barrier contraceptives during sex can help to reduce the risk of STIs. How soon after sex should you pee? There is no recommended time to pee after having sex, although some anecdotal sources suggest peeing within 30 minutes after sex. In general, the sooner people pee after sex, the sooner they can flush out bacteria before it travels up the urethra. If people are struggling to pee after sex, drinking a glass or two of water may help. A larger amount of urine will also be more effective in flushing out bacteria. Other ways to prevent UTIs The following tips may also help to reduce a person's risk of getting a UTI: drinking 8-10 glasses of water each day to ensure regular flushing of bacteria out of the urethra peeing whenever the urge arises, rather than holding in urine avoiding going more than 3 or 4 hours without urinating always wiping from front to back after going to the toilet cleaning the genitals with warm water each day avoiding using scented female hygiene products avoiding douching avoiding using spermicides if prone to UTIs wearing loose cotton underwear avoiding tight clothing avoiding staying in wet bathing or workout clothes that can trap moisture and harbor bacteria around the genitals limiting baths to 30 minutes or less, or taking showers drinking cranberry juice or taking cranberry extracts When to see a doctor People should see a doctor if they experience the following symptoms of a UTI: painful or burning sensation when urinating feeling the need to urinate often, despite passing only a small amount of urine each time cloudy urine foul-smelling urine blood in the urine pressure or pain in the lower abdomen feeling tired, weak, or shaky confusion If people have a UTI, a doctor will likely prescribe antibiotics to clear the infection. People will usually start feeling better within a few days. In some cases, a UTI can make its way up to the kidneys. A kidney infection can be severe and requires immediate medical treatment. Symptoms of a kidney infection include: a fever chills nausea vomiting pain in the lower back People should also see their doctor if they notice any unusual or painful symptoms during or after sex. These could be symptoms of an STI. Summary Peeing after sex may help to flush bacteria out of the urethra, thereby helping to prevent a urinary tract infection (UTI). It may be especially helpful for women, or people who are prone to UTIs. However, peeing after sex will not prevent pregnancy or sexually transmitted infections (STIs). People should see a doctor if they experience symptoms of a UTI or STI. Some people may require treatment with antibiotics. |
|
#255
|
||||
|
||||
|
Re: Sexual Health News
What to know about peeing after sex (Benefits)
Written by Beth Sissons on December 23, 2019 https://www.medicalnewstoday.com/art...eing-after-sex People may have heard that peeing after sex is beneficial, especially for women. This is because peeing flushes bacteria out of the body, which may help prevent a urinary tract from developing. Here, we look at how peeing after sex may help to prevent urinary tract infections. We also discuss whether there are any other benefits to peeing after sex. Benefits of peeing after sex Peeing after sex may reduce the risk of developing a UTI. Sexual intercourse is a risk factor for urinary tract infections (UTIs). During sex, bacteria can pass from the genitals to the urethra. The urethra is the tube that connects the bladder to the urethral opening where urine comes out. Bacteria can then make its way from the urethra to the bladder, resulting in a UTI. Peeing after sex helps to flush bacteria out of the urethra, helping to prevent UTIs. How can it help prevent UTIs? Females are up to 30 times more likely to get a UTI than males. This is due to two reasons: Firstly, the female urethra is close to the vagina and anus. This means that bacteria can easily spread from these areas to the urethra. Secondly, the urethra is shorter in females than it is in males. This means that bacteria that enter the urethra can reach the bladder more easily. In women, peeing after sex can help to flush any bacteria away from the urethra. For males, peeing after sex is less important. This is because males have a longer urethra. As a result, bacteria from the genital area is less likely to reach the bladder. Although there is no solid evidence to confirm that peeing after sex can prevent UTIs, there is no harm in following this practice. It may help to reduce the risk of UTIs, especially in women and people who are more prone to UTIs. Does it prevent pregnancy? Peeing after sex will not prevent pregnancy. The urethra and vagina are separate parts of the female anatomy. As a result, peeing will not affect any sperm that enter the vagina. Using some form of birth control is the only way to prevent pregnancy during sex. Does it prevent STIs? Peeing after sex does not prevent sexually transmitted infections (STIs). People contract STIs by absorbing bacteria through the mucous membranes inside their bodies during sexual intercourse. Peeing after sex will not prevent these bacteria from entering the body. Using a condom or other form of barrier contraceptives during sex can help to reduce the risk of STIs. How soon after sex should you pee? There is no recommended time to pee after having sex, although some anecdotal sources suggest peeing within 30 minutes after sex. In general, the sooner people pee after sex, the sooner they can flush out bacteria before it travels up the urethra. If people are struggling to pee after sex, drinking a glass or two of water may help. A larger amount of urine will also be more effective in flushing out bacteria. Other ways to prevent UTIs The following tips may also help to reduce a persons risk of getting a UTI: drinking 8-10 glasses of water each day to ensure regular flushing of bacteria out of the urethra peeing whenever the urge arises, rather than holding in urine avoiding going more than 3 or 4 hours without urinating always wiping from front to back after going to the toilet cleaning the genitals with warm water each day avoiding using scented female hygiene products avoiding douching avoiding using spermicides if prone to UTIs wearing loose cotton underwear avoiding tight clothing avoiding staying in wet bathing or workout clothes that can trap moisture and harbor bacteria around the genitals limiting baths to 30 minutes or less, or taking showers drinking cranberry juice or taking cranberry extracts When to see a doctor People should see a doctor if they experience the following symptoms of a UTI: painful or burning sensation when urinating feeling the need to urinate often, despite passing only a small amount of urine each time cloudy urine foul-smelling urine blood in the urine pressure or pain in the lower abdomen feeling tired, weak, or shaky confusion If people have a UTI, a doctor will likely prescribe antibiotics to clear the infection. People will usually start feeling better within a few days. In some cases, a UTI can make its way up to the kidneys. A kidney infection can be severe and requires immediate medical treatment. Symptoms of a kidney infection include: a fever chills nausea vomiting pain in the lower back People should also see their doctor if they notice any unusual or painful symptoms during or after sex. These could be symptoms of an STI. Summary Peeing after sex may help to flush bacteria out of the urethra, thereby helping to prevent a urinary tract infection (UTI). It may be especially helpful for women, or people who are prone to UTIs. However, peeing after sex will not prevent pregnancy or sexually transmitted infections (STIs). People should see a doctor if they experience symptoms of a UTI or STI. Some people may require treatment with antibiotics. |
| Advert Space Available |
 |
| Bookmarks |
|
|
 t Similar Threads
t Similar Threads
|
||||
| Thread | Thread Starter | Forum | Replies | Last Post |
| Non sexual health question | sicknasty | Sexual Health Issues | 7 | 10-01-2015 05:45 AM |
| Sexual Health Issues | Whybother | Sexual Health Issues | 2 | 24-04-2013 07:02 AM |
| DSC Sexual Health Screening | Huluman | Sexual Health Issues | 3 | 23-11-2008 08:57 PM |
| Sexual Health & Well Being | MrDevil | Sexual Health Issues | 10 | 29-03-2004 09:36 AM |
| sexual health mentor | boyrusty2000 | Sexual Health Issues | 31 | 06-08-2003 11:10 PM |